In an era where healthcare is increasingly patient-centric and preventative, the concept of self-care has risen to the forefront of medical and public health discourse. Self-care, encompassing the proactive steps individuals take to promote their health and wellbeing, is no longer considered a supplementary aspect of healthcare but a fundamental pillar in preventing and managing a wide array of conditions, including the growing burden of chronic non-communicable diseases. As the global healthcare landscape evolves, the ability to accurately and effectively assess an individual’s capacity for self-care becomes paramount. This need has spurred the development of various Self Care Assessment Tool For Patient Wellness, each aiming to quantify and qualify an individual’s self-care capabilities. However, the field remains fragmented, lacking a universally accepted, comprehensive tool that captures the multifaceted nature of self-care.
This article delves into the landscape of self care assessment tools for patient wellness, drawing upon a comprehensive review of existing instruments designed for adults. We explore the evolution of these tools, their underlying principles, and critically evaluate their strengths and limitations. Our aim is to highlight the critical need for a robust, validated, and easily accessible self care assessment tool that can truly empower both individuals and healthcare providers in the pursuit of holistic patient wellness. By understanding the current state of self-care assessment, we can pave the way for the development and implementation of more effective strategies to promote and support individual self-care practices, ultimately leading to improved health outcomes and a more sustainable healthcare system.
Decoding Self-Care: A Foundation for Patient Wellness
The World Health Organization (WHO) defines self-care as “the ability of individuals, families and communities to promote health, prevent disease, maintain health, and to cope with illness and disability with or without the support of a healthcare provider.” This broad definition underscores that self-care is not merely about treating illness but proactively engaging in practices that foster overall wellbeing. It encompasses a vast spectrum of behaviors and decisions, ranging from lifestyle choices and hygiene practices to environmental and socioeconomic considerations.
To provide a structured understanding of this broad concept, Webber and colleagues developed the “Seven Pillars of Self-Care” (7PSC) framework. This framework identifies seven essential domains that constitute comprehensive self-care:
- Knowledge and Health Literacy: Understanding health information and having the ability to make informed health decisions.
- Mental Wellbeing, Self-Awareness, and Agency: Maintaining positive mental health, recognizing one’s own needs, and feeling empowered to act on them.
- Physical Activity: Engaging in regular physical exercise to maintain physical health and fitness.
- Healthy Eating: Consuming a balanced and nutritious diet to support physical and mental health.
- Risk Avoidance and Mitigation: Taking steps to avoid or minimize health risks, such as smoking, excessive alcohol consumption, and unsafe behaviors.
- Good Hygiene: Practicing good personal hygiene to prevent infections and maintain overall health.
- Rational Use of Products and Services: Using health products and services appropriately and responsibly, including medications and healthcare resources.
This 7PSC framework provides a valuable benchmark for evaluating self-care practices across populations and serves as a foundation for assessing the comprehensiveness of self care assessment tools. Beyond these generic behaviors, self-care also includes condition-specific self-management practices for individuals with long-term conditions, such as adherence to medication regimens for diabetes or heart failure.
As healthcare systems globally grapple with increasing demands and resource constraints, self-care is increasingly recognized as a cornerstone of sustainable healthcare. Policymakers are actively investing in public health initiatives aimed at promoting self-care among the general population and self-management for those with chronic conditions. A crucial step in evaluating the effectiveness of these initiatives lies in accurately measuring an individual’s self-care capability. This is where the development and utilization of effective self care assessment tools for patient wellness become indispensable.
Navigating the Landscape of Self-Care Assessment Tools: A Scoping Review
To understand the current state of self care assessment tools for patient wellness, a comprehensive scoping review was undertaken to identify, evaluate, and map the various instruments available for adults. This review sought to characterize these tools in terms of their content, structure, and psychometric properties, providing a detailed analysis of their alignment with the 7PSC framework.
Methodology: A Systematic Search for Self-Care Measures
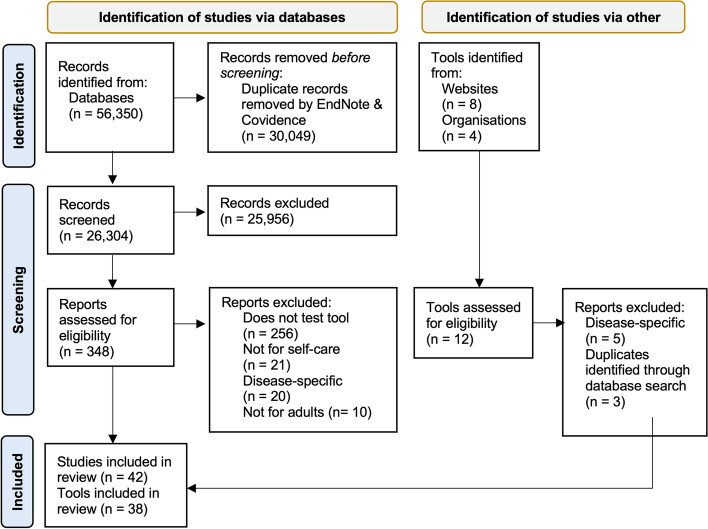
The scoping review adhered to the PRISMA extension for scoping reviews, ensuring a rigorous and transparent approach. A comprehensive search was conducted across major databases including Embase, PubMed, PsycINFO, and CINAHL, covering literature from 1950 to November 2022. The search strategy employed a combination of MeSH terms and keywords related to self-care, self-management, self-assessment, and measurement tools for adults.
Inclusion criteria were deliberately broad to capture a wide range of tools assessing health literacy, capability, and performance of general health self-care practices in adults. Tools focusing solely on disease-specific self-care or specific medical settings were excluded, ensuring the focus remained on general self care assessment tool for patient wellness. Both self-reported and observer-reported data collection methods were considered.
The study selection process involved rigorous screening of titles and abstracts, followed by full-text review by multiple researchers to ensure objectivity and consistency. Data extraction was performed using a standardized form, capturing key characteristics of each tool, including its description, origin, target population, number of items, scoring system, administration method, and reported psychometric properties.
A qualitative content assessment was conducted for each identified tool, utilizing the 7PSC framework as a guide. This assessment aimed to determine the extent to which each tool captured information relevant to each of the seven pillars of self-care. A Black, Red, Amber, and Green (BRAG) traffic light system was used to visually represent the alignment of each tool with the 7PSC framework, allowing for a clear and comparative analysis.
Key Findings: A Diverse but Incomplete Toolkit
The review identified 38 distinct self care assessment tools described in 42 primary reference studies. These tools exhibited considerable diversity in their origins, target populations, and assessment approaches.
Geographical Distribution and Target Populations: The majority of tools originated from North America (primarily the USA), with a smaller representation from European countries and international collaborations. While a significant portion of tools (63.2%) were designed for general health and self-care assessment, a substantial number (36.8%) were tailored to specific populations, including the elderly, in-patients, individuals with chronic illnesses or disabilities, and those with psychiatric disorders. This highlights the varying contexts in which self care assessment tools are utilized.
Tool Length and Data Collection Methods: The length of the tools varied considerably, ranging from a brief 5-item questionnaire (EQ-5D) to a comprehensive 121-item interview (SFS). The average tool length was 34.4 items. Data collection methods also differed, with some tools relying on staff or observer completion (28.9%), others designed for self-administration (52.6%), and some offering adaptable versions (15.8%). This reflects a shift over time from observer-based assessments towards self-reporting, empowering individuals in the assessment process.
Scoring Systems and Time Burden: The scoring systems were predominantly numerical integer rating scales, with most tools summing item scores to generate a total score reflecting self-care ability. However, the interpretation of scores varied, with some tools indicating higher scores as better self-care, while others interpreted higher scores as poorer self-care practices. Information on the time required to complete the tools was often lacking (63.2% of tools). For those reporting completion time, the average ranged from 2 to 30 minutes, with an estimated average of 12.8 minutes across all tools.
Psychometric Properties and Theoretical Underpinnings: Encouragingly, a high percentage of tools reported evidence of validity (94.7%) and reliability (92.1%) in published studies. However, the theoretical underpinnings of the tools were less consistent. While some tools (21.1%) explicitly utilized Orem’s Theory of Self-Care, a significant number (47.4%) lacked a clearly defined theoretical framework. This suggests a potential gap in the conceptual rigor of some self care assessment tool for patient wellness.
Evolution of Self-Care Assessment: A temporal analysis revealed a significant shift in the focus of self care assessment tools over time. Earlier tools were predominantly geared towards chronic disease management and rehabilitation, reflecting a more passive view of patients as recipients of care. However, a notable transition occurred in the late 1980s towards prevention-focused tools, aligning with the growing emphasis on individual responsibility for health and the rise of lifestyle medicine. This evolution mirrors the broader shift in healthcare towards proactive prevention and patient empowerment. Similarly, the method of administration has transitioned from observer-reported to self-reported assessments, further emphasizing patient involvement in the self-care evaluation process.
7PSC Framework Analysis: Gaps in Comprehensive Coverage
The content assessment against the 7PSC framework revealed significant insights into the comprehensiveness of existing self care assessment tools. While the tools collectively covered a wide range of self-care practices, their coverage of the seven pillars was uneven.
Pillars Adequately Represented: Physical activity, mental wellbeing, and knowledge and health literacy emerged as the most frequently addressed pillars. This suggests that current tools tend to emphasize these aspects of self-care.
Pillars Underrepresented: Risk avoidance and mitigation, and the rational use of products and services were less consistently represented across the tools. Notably, healthy eating and good hygiene, fundamental aspects of self-care, were among the least represented pillars. This highlights a potential blind spot in current self care assessment tool for patient wellness, particularly concerning basic health behaviors.
Limited Comprehensive Tools: Crucially, only five out of the 38 tools included questions relevant to all seven pillars of self-care. This striking finding underscores the lack of comprehensive self care assessment tools that truly capture the multifaceted nature of self-care as defined by the 7PSC framework.
This image illustrates the systematic process used to identify relevant self-care assessment tools for the scoping review, highlighting the rigorous approach taken to ensure comprehensive coverage of the literature.
Discussion: Towards a More Holistic Approach to Self-Care Assessment
The findings of this scoping review underscore the critical need for a more holistic and comprehensive approach to self care assessment tool for patient wellness. While a diverse range of tools exists, few adequately capture the full spectrum of self-care practices as defined by the 7PSC framework.
Key Trends and Implications
Shift Towards Patient-Centricity: The evolution towards self-reported data collection methods reflects a broader trend towards patient-centered care and the recognition of individuals as active participants in their own health journeys. This shift is positive, empowering individuals and potentially reducing the burden on healthcare professionals. However, it also necessitates careful consideration of potential biases in self-reported data and the need for robust validation of self-report measures. Mixed-methods approaches, incorporating both self-report and observer input, may offer a balanced and comprehensive assessment in the future.
From Management to Prevention: The temporal shift from rehabilitation-focused to prevention-focused tools reflects the growing recognition of the importance of preventative healthcare and lifestyle medicine. This evolution is crucial as healthcare systems increasingly prioritize prevention to address the rising burden of chronic diseases and promote long-term patient wellness. Self care assessment tools designed for prevention can play a vital role in identifying individuals at risk and tailoring interventions to promote healthy behaviors proactively.
The Neglected Pillars: The underrepresentation of pillars such as healthy eating, good hygiene, risk avoidance, and rational use of products in many self care assessment tools is concerning. These pillars represent fundamental aspects of self-care that directly impact patient wellness. The relative neglect of hygiene, despite its foundational role in public health, is particularly noteworthy and warrants renewed attention. In the modern context, hygiene should also encompass digital hygiene practices, reflecting the impact of technology on health and wellbeing.
The Need for a Unifying Framework: The lack of a universally accepted, comprehensive self care assessment tool highlights the need for a unifying framework to guide the development and standardization of future instruments. Such a framework should ideally be grounded in a robust theoretical model of self-care, such as the 7PSC framework, and encompass all key domains relevant to patient wellness.
Implications for Research, Policy, and Practice
Research: Future research should prioritize the development and validation of comprehensive self care assessment tools that address all seven pillars of self-care. This includes rigorous psychometric testing, standardization of scoring and administration methods, and exploration of mixed-methods approaches. Furthermore, research is needed to develop culturally appropriate tools and validate existing tools in diverse populations, considering factors such as language, literacy, and cultural norms.
Policy: Policymakers should recognize the critical role of self-care assessment in promoting patient wellness and supporting public health initiatives. Investing in the development and implementation of validated self care assessment tools can inform targeted interventions, evaluate the effectiveness of self-care promotion programs, and contribute to a more sustainable and patient-centered healthcare system.
Practice: Healthcare providers can utilize existing self care assessment tools to gain valuable insights into their patients’ self-care capabilities. However, it is crucial to be aware of the limitations of current tools, particularly their potential lack of comprehensiveness. In practice, a more holistic approach to self-care assessment may involve combining existing tools with clinical judgment and patient-centered conversations to gain a more complete understanding of individual self-care needs and strengths. The routine use of a validated and comprehensive self care assessment tool for patient wellness can guide the delivery of tailored health and social care interventions, ultimately empowering patients to take greater ownership of their health and wellbeing.
Conclusion: Charting a Course for Enhanced Patient Wellness Through Self-Care Assessment
This scoping review provides a comprehensive overview of the landscape of self care assessment tools for patient wellness. While a diverse array of tools exists, a significant gap remains in the availability of comprehensive, validated instruments that capture the multifaceted nature of self-care. The review highlights the evolution of self-care assessment, the strengths and limitations of current tools, and the critical need for a more holistic and standardized approach.
Moving forward, the development of a comprehensive self care assessment tool based on a unifying framework like the 7PSC is paramount. Such a tool should be rigorously validated, easily accessible, and culturally appropriate for diverse populations. It should encompass all seven pillars of self-care, providing a holistic assessment of individual capabilities and informing targeted interventions to promote patient wellness. The ongoing development of tools like the Self-Care CAPabiIity AssessmeNt (CAPITAN) Toolkit, grounded in the 7PSC framework, represents a promising step in this direction.
By prioritizing the development and implementation of effective self care assessment tools, we can empower individuals, healthcare providers, and policymakers to work collaboratively towards a future where self-care is not just a concept but a measurable and achievable reality, leading to enhanced patient wellness and a more sustainable healthcare ecosystem. The journey towards truly patient-centered and preventative healthcare hinges on our ability to accurately assess and effectively support individual self-care capabilities, and comprehensive self care assessment tools are indispensable instruments on this path.
This table visually summarizes the alignment of various self care assessment tools with the 7PSC framework, providing a comparative overview of their strengths and weaknesses in covering different domains of self-care. It underscores the variability in comprehensiveness among existing tools and highlights the need for more holistic instruments.