Introduction
Despite advancements in cancer treatments, the global burden of cancer deaths remains significant, highlighting the crucial need for effective palliative care (PC). International guidelines advocate for early integration of PC for cancer patients, ideally alongside active treatments, to improve quality of life and survival rates. However, efficiently identifying patients who would benefit most from palliative care referral remains a challenge, particularly within busy comprehensive cancer centers. The PALLIA-10 questionnaire, developed by the French Society for Palliative Support and Care (SFAP), is a 10-item screening tool designed to aid healthcare professionals in identifying patients in need of palliative care. This study investigates the practical application and effectiveness of the PALLIA-10 questionnaire and its associated scoring system as a Screening Tool For Palliative Care Referrals in advanced cancer patients within comprehensive cancer centers. This research aims to determine the optimal PALLIA-10 score threshold for effective referral in this specific setting.
Methods
This prospective, multicenter study, known as PREPA-10, was conducted across 18 French comprehensive cancer centers. Hospitalized adult patients from medical oncology and radiotherapy departments were enrolled on a single designated day in each center. Patients in surgical units and outpatients were excluded from this study focused on inpatient palliative care needs. The study was approved by relevant French ethical and regulatory bodies (CCTIRS, CNIL, Ethic committee Lyon Sud-Est IV) and registered on ClinicalTrials.gov (NCT02479061).
Data collected included patient demographics, disease characteristics, reason for hospitalization, and current palliative care management status. The PALLIA-10 questionnaire was administered to patients deemed to have incurable disease. Healthcare teams, including physicians and nurses, were trained on the standardized use of the PALLIA-10 questionnaire and scoring. The PALLIA-10 score ranges from 0 to 10, assessing medical, psychosocial, and ethical dimensions relevant to palliative care needs. Patient recruitment occurred on a single day at each site to ensure a point-prevalence evaluation. Disease stage was classified using the Krakowski classification to define palliative settings. Patient survival data were tracked for six months post-study to assess overall survival and palliative care referral rates.
Results
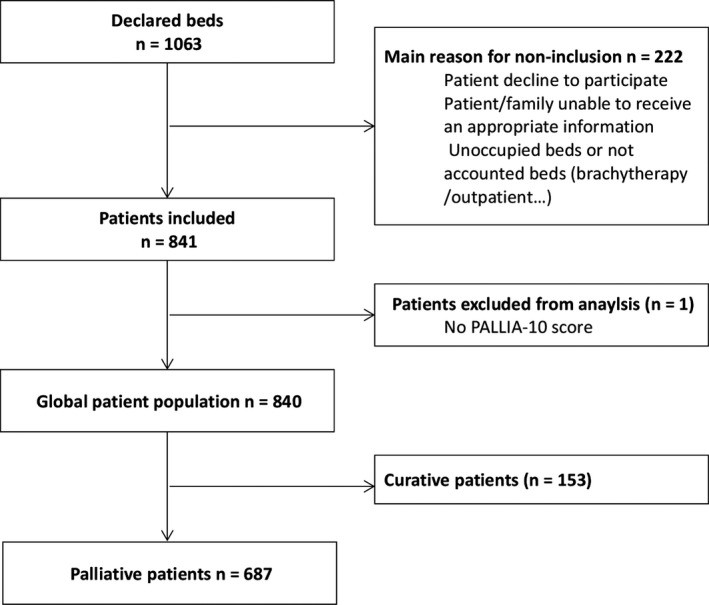
A total of 840 patients were enrolled, with 687 (82%) identified as being in a palliative setting. Among these palliative patients, 479 (69.5%) had a PALLIA-10 score greater than 3, and 230 (33.5%) scored greater than 5. At the time of the study, 216 (31.4%) patients were already receiving palliative care services. Within six months following the study, an additional 152 patients were referred to palliative care.
Figure 1: Trial profile illustrating patient enrollment and categorization in the PREPA-10 study, highlighting the focus on palliative care patients.
The PALLIA-10 score demonstrated a significant association with palliative care referral. Logistic regression analysis showed that patients with a PALLIA-10 score greater than 3 were significantly more likely to be referred to palliative care (adjusted OR 2.6, 95%CI 1.65-4.11). Further analysis revealed even stronger associations for higher scores: patients with scores of 4-5 had an adjusted OR of 1.9 (95%CI 1.17-3.16), and those with scores greater than 5 had an adjusted OR of 3.59 (95%CI 2.18-5.91). These findings indicate that higher PALLIA-10 scores are strong predictors of palliative care intervention.
Survival analysis also demonstrated the prognostic value of the PALLIA-10 score. Median overall survival was significantly shorter for patients with higher PALLIA-10 scores. Patients with scores between 4 and 5 had a median OS of 2.6 months (95%CI 2.1-3.2), and those with scores greater than 5 had a median OS of 1.3 months (95%CI 0.95-1.7), compared to patients with scores ≤3 who had a not reached median OS during the study period. Multivariate Cox regression confirmed the PALLIA-10 score as an independent prognostic factor for overall survival, even after adjusting for other known prognostic variables such as Karnofsky index and number of metastatic sites. Specifically, patients with PALLIA-10 scores between 4 and 5 had a hazard ratio (HR) for death of 1.58 (95%CI 1.20-2.08), and those with scores greater than 5 had an HR of 2.18 (95%CI 1.63-2.92).
Figure 2: Distribution of PALLIA-10 scores within the palliative patient population, illustrating the range and frequency of scores obtained in the study.
Figure 3: Palliative care intervention distribution in relation to PALLIA-10 scores, showing the proportion of patients receiving palliative care at different score thresholds.
Figure 4: Kaplan-Meier survival curves demonstrating overall survival differences across PALLIA-10 score categories, highlighting the prognostic capability of the tool.
Discussion
The PREPA-10 study is the first large-scale, prospective, multicenter investigation to evaluate the PALLIA-10 questionnaire as a screening tool for palliative care referrals in hospitalized cancer patients. The study’s findings strongly support the use of PALLIA-10 as a practical and efficient instrument for identifying inpatients who require palliative care within comprehensive cancer centers. The ease of use and rapid scoring of the questionnaire make it readily integrable into routine hospital workflows, facilitating communication among healthcare teams. The broad participation of French cancer centers enhances the generalizability of these results within similar healthcare systems.
While the SFAP recommended a PALLIA-10 score threshold of >3 for palliative care referral, our results suggest that a higher threshold, specifically >5, might be more appropriate in the context of advanced cancer patients in comprehensive cancer centers. Using a threshold of >3 would identify a large proportion of patients (approximately 70%) for referral, potentially overwhelming existing palliative care resources. The ROC analysis in our study further supports a cut-off point of 5 for optimal sensitivity and specificity in identifying patients most likely to benefit from palliative care.
The PALLIA-10 questionnaire’s strength lies in its multidimensional approach, encompassing not only clinical and biological factors but also crucial psychosocial and ethical considerations. This holistic assessment aligns with the philosophy of palliative care, addressing the complex needs of patients facing advanced cancer. The study demonstrates that this multidimensional assessment is not only clinically relevant but also statistically robust, providing a valuable tool for decision-making in palliative care.
The PALLIA-10 score’s predictive value for palliative care intervention and its prognostic significance for overall survival underscore its utility as both a screening tool for palliative care referrals and a valuable indicator of patient prognosis. However, it is important to acknowledge the limitations of this study. The focus on hospitalized patients in French comprehensive cancer centers may limit the generalizability of the findings to other settings, such as outpatient clinics or different healthcare systems. Further research is needed to evaluate the PALLIA-10 in diverse populations and care settings.
Conclusion
The PALLIA-10 questionnaire is a valuable and easily implemented screening tool for palliative care referrals for cancer inpatients in comprehensive cancer centers. While the currently recommended threshold of >3 may be too sensitive for resource allocation in this setting, a threshold of >5 appears more pragmatic for identifying patients with the most pressing palliative care needs. Implementing the PALLIA-10 questionnaire can facilitate timely palliative care referrals, potentially improving patient outcomes and quality of life. Future research should focus on the impact of PALLIA-10 implementation on patient-reported outcomes, quality of life, and caregiver burden, as well as exploring the qualitative contributions of the questionnaire’s individual items, particularly the psychosocial components, to optimize its application in diverse clinical contexts.
Conflict of Interest
The authors declare no conflict of interest.