The Safer Nursing Care Tool (SNCT) was widely adopted in English hospitals in 2016 to determine appropriate nurse staffing levels. This study examines the tool’s precision in estimating staffing requirements and its correlation with nurses’ professional judgment regarding adequate staffing.
Estimating Nurse Staffing Requirements with the SNCT
The SNCT, a patient classification system, assigns patients to categories based on their acuity and dependency. Each category has a corresponding weighting (“multiplier”) reflecting the required nursing staff. The study analyzed data from 81 medical/surgical units in four English hospitals, encompassing over 22,000 unit days.
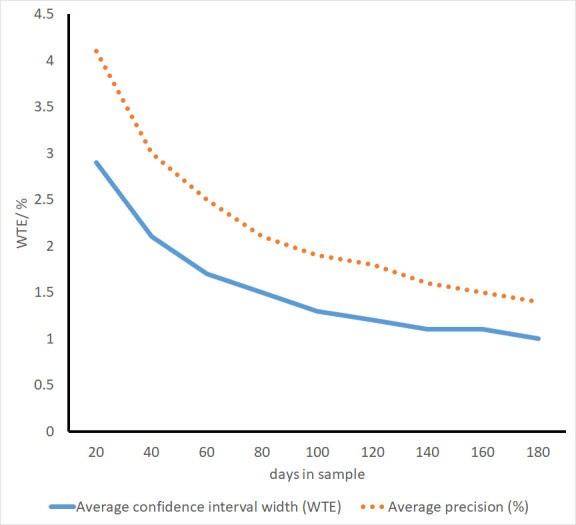
The recommended minimum sample size of 20 days yielded an average precision of 4.1% in estimating the required staffing establishment. However, this translated to wide confidence intervals (CIs) in terms of absolute staff numbers, often exceeding ±1.5 whole-time equivalent (WTE) staff members.
Correlation Between SNCT Estimates and Professional Judgment
The study investigated the relationship between staffing shortfalls, as identified by the SNCT, and nurses’ perceptions of staffing adequacy. Nurses reported whether there were enough staff for quality care, if necessary care was left undone, and if staff missed breaks.
Results showed a strong correlation: for each registered nurse hour shortfall per patient day (HPPD), the odds of nurses reporting sufficient staff for quality decreased by 11%. Similarly, the odds of reporting missed necessary care and missed breaks increased by 14% and 12%, respectively. These relationships were linear, with no evidence of a staffing threshold where the impact on perceived adequacy diminished.
Factors Beyond the SNCT Affecting Staffing Adequacy
The study also revealed that factors not explicitly considered in the SNCT influenced staffing perceptions. Nurses in surgical units were less likely to report adequate staffing compared to those in medical or mixed units. Although not statistically significant, units with a higher proportion of single rooms and higher patient turnover also tended toward lower staffing adequacy perceptions.
Conclusion: The SNCT as a Tool, Not a Replacement for Judgment
The 2016 analysis of the SNCT demonstrated its ability to provide a reliable measure of nursing workload. Larger sample sizes than the recommended minimum (20 days) significantly improved precision in estimating staffing establishments. However, the study highlighted that the SNCT-recommended staffing levels might not be universally optimal, as the relationship between staffing levels and perceived adequacy remained linear even above recommended levels.
Factors like surgical specialty, patient turnover, and the proportion of single rooms—not directly accounted for in the SNCT—also impacted perceived staffing adequacy. Therefore, while the SNCT served as a valuable tool for assessing workload and guiding staffing decisions, it could not replace professional nursing judgment in ensuring safe and effective patient care. The SNCT provided a framework, but experienced nurses remained crucial in interpreting the data and adjusting staffing levels to meet the dynamic demands of their specific units.