Point-of-care (POC) tools are essential resources for nurses seeking evidence-based information to inform patient care decisions. This article examines the evaluation of five prominent POC tools using a rubric designed specifically for nursing practice needs. The rubric assesses content, coverage of nursing topics, evidence transparency, user perception, and customization options. The findings highlight the strengths and weaknesses of each tool, ultimately guiding informed decision-making for healthcare institutions and professionals.
Evaluating Content and Nursing Coverage in POC Tools
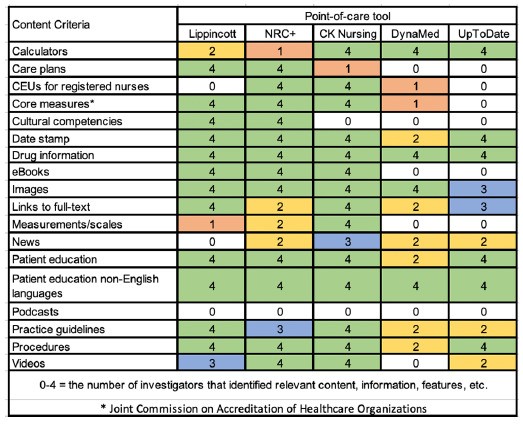
Five POC tools were evaluated: ClinicalKey for Nursing, DynaMed, Lippincott’s Advisor and Procedures, Nursing Reference Center Plus, and UpToDate. The evaluation rubric focused on the presence of diverse content types relevant to nursing practice, such as care plans, patient education materials, and continuing education opportunities. While all tools offered some nursing-related content, specialized nursing POC tools (ClinicalKey for Nursing, Lippincott’s Advisor and Procedures, and Nursing Reference Center Plus) provided a broader range of resources tailored to bedside nurses’ needs.
ClinicalKey for Nursing excelled in content related to interventions and outcomes, while Lippincott’s Advisor and Procedures demonstrated comprehensive coverage of diagnoses. Nursing Reference Center Plus offered the most well-rounded coverage of nursing terminology and topics. However, DynaMed and UpToDate, while strong in medical information, lacked comprehensive coverage of nursing-specific content.
Transparency and Customization: Key Considerations for POC Tool Selection
Transparency in evidence presentation and potential bias disclosure is crucial for informed decision-making. DynaMed demonstrated the highest transparency, consistently providing information on evidence currency, grading methods, and conflict of interest policies. UpToDate also performed well in this area. Conversely, the nursing-focused POC tools lacked clear transparency regarding evidence sources and potential biases.
Customization options, enabling users to personalize their experience and streamline workflows, varied significantly across the tools. DynaMed and Nursing Reference Center Plus offered more robust customization features, such as saving content, setting alerts, and offline access via mobile apps. However, limitations in customization were noted across several platforms, hindering the ability to tailor resources to individual user needs and institutional preferences.
Conclusion: Informing POC Tool Selection for Optimal Nursing Practice
This evaluation revealed that no single POC tool fully met all criteria for optimal nursing practice. Each tool possessed unique strengths and weaknesses, highlighting the importance of a thorough assessment based on specific institutional and user requirements. For comprehensive coverage, a combination of a specialized nursing POC tool and a broader medical resource like DynaMed or UpToDate may be necessary.
Ultimately, the selection of a POC tool should prioritize content relevance, evidence transparency, user-friendliness, and customization options to ensure that nurses have access to the most accurate and actionable information for delivering high-quality patient care. Future research involving direct user feedback from nurses will further enhance the understanding of POC tool effectiveness and inform future development in this crucial area.