Introduction
In today’s dynamic healthcare environment, nurses at the point of care (POC) are pivotal in delivering exceptional patient outcomes. Implementing evidence-based practices (EBPs) is crucial for ensuring safe, effective, and patient-centered care. However, the successful adoption of EBPs often hinges on effective leadership at the POC. While the importance of leadership in driving change is widely recognized, the specific leadership behaviors and tools that foster EBP implementation in nursing are increasingly coming into focus. This article delves into the concept of implementation leadership (IL) and explores practical tips and tools for nurses to enhance their leadership capabilities at the point of care, drawing insights from recent research evaluating measures of implementation leadership in nursing.
Understanding Point of Care Leadership in Nursing
Point of care nursing leadership is multifaceted, encompassing various roles beyond traditional nurse managers. Nurses in advanced practice roles, such as clinical nurse specialists and nurse practitioners, alongside nursing professional development educators and nurse champions, all contribute to leadership at the POC. These roles share the common expectation of improving patient care, advancing nursing practice, and guiding local implementation efforts.
Key Point of Care Nurse Leader Roles:
- Nurse Managers: Oversee daily operations, resource allocation, and team performance, directly influencing EBP adoption through policy and support.
- Advanced Practice Nurses (APNs): Clinical Nurse Specialists and Nurse Practitioners lead in specialized areas, championing best practices and mentoring staff in EBP implementation.
- Nursing Professional Development Educators: Facilitate learning and competency building, equipping nurses with the knowledge and skills to implement EBPs effectively.
- Nurse Champions: Passionate advocates for change, driving EBP adoption through peer influence, education, and acting as role models.
These POC nurse leaders utilize a mix of strategies, both directive and enabling, to guide their nursing teams in embracing EBPs. Their approach is often shaped by their formal authority and the specific context of their roles, emphasizing the need for adaptable and effective leadership behaviors.
The Significance of Implementation Leadership
Implementation leadership (IL) has emerged as a critical concept in implementation science, highlighting the specific behaviors leaders enact to promote the successful integration of EBPs. IL goes beyond general leadership qualities, focusing on the unique skills and knowledge leaders need to effectively facilitate implementation. These include:
- General Leadership Abilities: Foundational skills in communication, team building, and problem-solving.
- Identifying EBP Gaps: Recognizing areas where current practices can be improved by adopting EBPs.
- Setting Clear Goals: Establishing measurable objectives for EBP implementation initiatives.
- Strategic Selection of Implementation Strategies: Choosing the most appropriate methods to facilitate EBP adoption within their specific setting.
- Active Engagement of Staff: Involving and motivating nursing staff throughout the implementation process.
Research increasingly links unit nurse managers’ IL behaviors to positive implementation climates. A supportive implementation climate is characterized by a shared perception among staff that EBPs are valued, encouraged, and expected within their environment. This climate acts as a crucial mediator, significantly influencing the successful uptake and sustained use of EBPs.
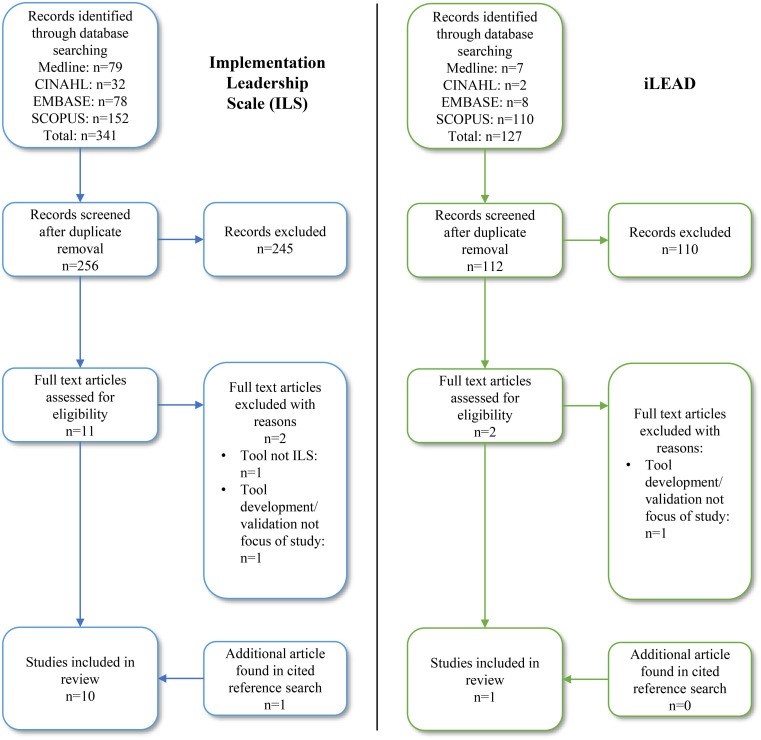
Tools for Assessing Implementation Leadership: ILS and iLEAD
To effectively measure and develop implementation leadership capacity in nursing, validated and reliable assessment tools are essential. Currently, two primary tools designed to measure IL are the Implementation Leadership Scale (ILS) and the iLEAD. A recent systematic review rigorously examined these tools to determine their suitability and psychometric properties for use in nursing contexts.
The Implementation Leadership Scale (ILS):
The ILS is designed to measure key dimensions of implementation leadership through 12 items across four subscales:
- Proactive Leadership: Reflects a leader’s initiative in planning and driving implementation.
- Knowledgeable Leadership: Assesses a leader’s understanding of EBPs and the implementation process.
- Supportive Leadership: Measures the extent to which a leader provides resources, encouragement, and removes barriers to EBP implementation.
- Perseverant Leadership: Evaluates a leader’s persistence and commitment to overcoming challenges during implementation.
The ILS is available in both leader self-report and staff report versions, offering flexibility in assessing IL from different perspectives. The review indicated that the ILS shows promise for use in nursing, demonstrating good structural validity and internal consistency in nursing contexts. It has also been adapted and validated in different languages, increasing its accessibility.
The iLEAD:
The iLEAD tool assesses implementation leadership based on active and passive leadership domains, drawing from the Full Range Leadership Model. It contains 16 items across two main factors:
- Active Implementation Leadership: Encompasses exemplary behaviors, individualized consideration, intellectual stimulation, and contingent reward.
- Passive Implementation Leadership: Reflects a more hands-off or reactive approach to leadership.
While the iLEAD has demonstrated good psychometric properties, the review suggests that the ILS may be more directly applicable to nursing due to its validation within hospital-based nursing settings and its alignment with models informed by nursing practice.
Choosing the Right Tool:
For nurses seeking to assess and develop implementation leadership at the POC, the ILS currently appears to be a more contextually relevant and promising tool. Its focus on proactive, knowledgeable, supportive, and perseverant leadership behaviors directly translates to actionable areas for development in nursing leadership.
PRISMA flow diagram illustrating the systematic review process for evaluating implementation leadership measurement tools.
Practical Tips for Point of Care Nurse Leaders Based on Implementation Leadership Principles
Drawing from the dimensions of implementation leadership and the findings of the tool review, here are practical tips for nurses to enhance their leadership at the point of care:
1. Be Proactive in Implementation:
- Develop a Clear Plan: Outline specific steps, timelines, and responsibilities for EBP implementation initiatives.
- Anticipate and Address Barriers: Proactively identify potential challenges and develop strategies to mitigate them.
- Communicate Vision Early and Often: Clearly articulate the benefits of EBPs and the implementation goals to your team from the outset.
2. Demonstrate Knowledgeable Leadership:
- Stay Updated on EBPs: Continuously seek out and share current evidence-based guidelines and research relevant to your practice area.
- Become an EBP Resource: Develop your expertise in EBPs and serve as a knowledgeable resource for your team, answering questions and providing guidance.
- Facilitate EBP Education: Organize workshops, in-services, or journal clubs to enhance your team’s understanding of EBPs.
3. Provide Supportive Leadership:
- Create a Psychologically Safe Environment: Encourage open communication, feedback, and questions about EBP implementation without fear of judgment.
- Offer Resources and Training: Ensure your team has access to the necessary tools, training, and support to implement EBPs effectively.
- Recognize and Reward Efforts: Acknowledge and celebrate both individual and team successes in EBP implementation to foster motivation and reinforce positive behaviors.
4. Embrace Perseverant Leadership:
- Maintain Commitment Through Challenges: Expect setbacks and challenges during implementation and demonstrate unwavering commitment to the process.
- Problem-Solve and Adapt: Be prepared to adjust implementation strategies as needed, learning from challenges and adapting your approach.
- Foster a Culture of Continuous Improvement: Encourage a mindset of ongoing evaluation and refinement of practices, viewing implementation as an iterative process.
5. Utilize Assessment Tools for Self-Reflection and Team Development:
- Consider Using the ILS: Employ the Implementation Leadership Scale to assess your own leadership behaviors and identify areas for growth.
- Facilitate Team Assessments: Use staff report versions of the ILS to gather feedback from your team on leadership effectiveness and identify team-level development needs.
- Use Assessment Data for Targeted Development: Utilize the insights from IL assessments to guide leadership development activities, mentorship, and team training initiatives.
Integrating Implementation Leadership into Nursing Practice
To truly embed implementation leadership within nursing practice, a multi-faceted approach is needed:
- Leadership Development Programs: Incorporate IL competencies and tools into nursing leadership training programs at all levels.
- Mentorship and Coaching: Pair experienced nurse leaders with emerging leaders to provide guidance and support in developing IL skills.
- Team-Based Leadership Models: Foster shared leadership approaches within nursing teams, recognizing and leveraging the diverse leadership contributions of all team members.
- Organizational Support for EBP: Create an organizational culture that values and supports EBP implementation, providing resources and infrastructure to enable effective leadership at the POC.
Conclusion
Effective point of care leadership is indispensable for driving the successful implementation of evidence-based practices in nursing and ultimately enhancing patient care. By understanding the principles of implementation leadership and utilizing tools like the ILS, nurses can strategically develop their leadership skills, foster supportive implementation climates, and lead their teams in adopting and sustaining EBPs. Focusing on proactive, knowledgeable, supportive, and perseverant leadership behaviors, combined with continuous self-reflection and team development, will empower nurses to excel as point of care leaders and champions of evidence-based practice, leading to improved outcomes for both patients and the nursing profession.