Patient-centered care is fundamental in family medicine, prioritizing the patient’s experience and needs. This article delves into the crucial aspect of assessing patient perception of care, examining various tools and instruments available to measure this vital component of healthcare quality. Understanding how patients perceive their care is essential for improving healthcare delivery, fostering stronger doctor-patient relationships, and ultimately enhancing health outcomes. This review provides a comprehensive analysis of existing measurement tools, focusing on their applicability and effectiveness in capturing patient perception of care within family medicine settings.
The Significance of Patient Perception in Patient-Centered Care
The concept of patient-centered care has evolved significantly since its inception, rooted in the humanistic psychology of Carl Rogers and further developed in medicine by Michael Balint. Today, it stands as a cornerstone of family medicine, recognized for its positive impact on various aspects of healthcare. Patient-centered care has been linked to reduced malpractice claims, increased physician satisfaction, improved consultation experiences, better patient emotional well-being, and enhanced medication adherence. Moreover, it can empower patients, reduce symptom severity, optimize healthcare resource utilization, and potentially lower healthcare costs.
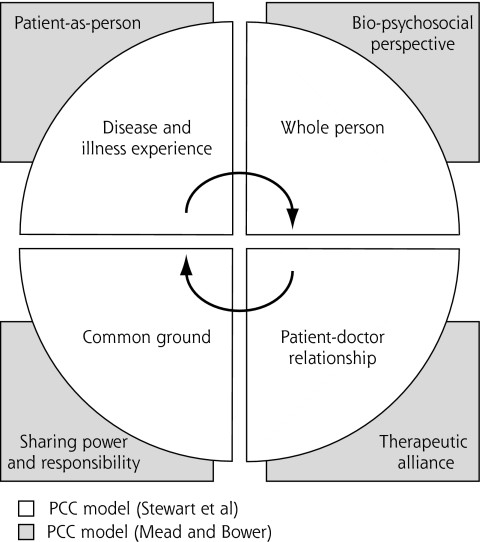
While the importance of patient-centered care is widely acknowledged, its definition can vary. The model proposed by Stewart and colleagues, emphasizing dimensions such as exploring both disease and illness, understanding the whole person, finding common ground, incorporating prevention, enhancing the doctor-patient relationship, and being realistic, is frequently cited in family medicine. Mead and Bower further refined this concept by identifying key dimensions within the doctor-patient relationship: a biopsychosocial perspective, viewing the patient as a person, shared power and responsibility, therapeutic alliance, and recognizing the doctor as a person.
For effective measurement, a clear conceptual framework is paramount. This review adopts a framework built upon four core dimensions common to both Stewart et al. and Mead and Bower’s models: (1) disease and illness experience, (2) the whole person perspective, (3) establishing common ground, and (4) the patient-doctor relationship. This framework serves as the foundation for evaluating and comparing instruments designed to measure patient perception of care.
Figure 1. Conceptual Framework of Patient-Centered Care (PCC)
Measuring patient-centered care can be approached through various methodologies, including direct observation and self-assessment questionnaires. Notably, studies indicate that patient perception measures are more predictive of positive outcomes compared to observations or physician perceptions. Experts advocate for patient-administered questionnaires as the most effective method for gauging patient-centered care attributes in primary healthcare settings. This review focuses specifically on instruments designed to assess patient perceptions of patient-centered care within family medicine.
Methodology for Identifying Patient Perception Measurement Tools
This systematic review adhered to rigorous standards, drawing upon guidelines established by the Agency for Healthcare Research and Quality.
Inclusion Criteria for Tool Selection
The review included articles that met specific criteria: (1) describing self-administered instruments that measured at least two dimensions of the established patient-centered care conceptual framework, (2) reporting quantitative or psychometric findings related to instrument development or validation, and (3) relevant to ambulatory family medicine contexts.
Literature Search and Study Selection Process
A comprehensive electronic literature search was conducted across MEDLINE, Embase, and Cochrane databases, covering the period from 1980 to April 2009. The search strategy, developed with an information specialist, utilized MeSH terms and keywords such as “patient-centered care,” “questionnaire,” “process assessment (health care),” and related terms. The search was broadened to include terms like “family practice” and “primary health care” in conjunction with “patient-centered care.”
Manual searching of reference lists and expert consultations further supplemented the electronic search to identify additional relevant articles. All identified references were managed in Refworks to remove duplicates. Initial screening of titles and abstracts was performed, followed by full-text reviews by two independent authors to determine final eligibility. Discrepancies were resolved through team consensus.
Quality Assessment of Selected Studies
The quality of included studies was evaluated using a modified version of the Standards for Reporting of Diagnostic Accuracy (STARD). This 15-item scale assessed various aspects of study methodology and reporting. Two researchers independently scored each article, and any differences were resolved through discussion. Studies scoring below 8 out of 15 were excluded to ensure the inclusion of methodologically sound research.
Data Extraction and Synthesis
For each instrument, data were extracted on development procedures, conceptual basis, quality score, instrument description (dimensions and items), response scale, and reported psychometric properties (internal consistency, test-retest reliability, predictive validity). Data extraction was performed independently by two team members, and disagreements were resolved through consensus.
Instrument items and subscales were mapped to the dimensions of the patient-centered care conceptual framework. An item-level analysis was conducted to accurately reflect the alignment of instrument components with the framework dimensions.
Review Findings: Instruments for Assessing Patient Perception of Care
The literature search and selection process yielded 26 articles, covering 13 distinct instruments, that met the inclusion criteria.
Overview of Included Instruments
Figure 2 illustrates the article selection process. The quality scores of the included articles ranged from 8 to 14 out of a possible 15, indicating a generally good methodological quality.
Figure 2. Article Selection Process for Systematic Review
Of the instruments reviewed, two were specifically designed to measure patient-centered care: the Patient Perception of Patient-Centeredness (PPPC) and the Consultation Care Measure (CCM). The remaining eleven instruments included subscales or items relevant to patient-centered care, although they were initially developed to assess broader aspects of healthcare.
Dedicated Patient-Centered Care Instruments: PPPC and CCM
Patient Perception of Patient-Centeredness (PPPC): Developed in Canada, the PPPC is grounded in Stewart et al.’s model and empirical research on doctor-patient relationships. It comprises 14 items using a 4-point Likert scale and assesses patient perceptions of patient-centeredness during a recent family physician visit. The PPPC demonstrated good internal consistency (Cronbach’s α = .71) and showed correlations with positive health outcomes, such as better recovery and emotional health, as well as reduced diagnostic testing and referrals. It effectively measures the dimensions of disease and illness experience, whole person perspective, and common ground.
Consultation Care Measure (CCM): Developed in the UK, the CCM is also based on Stewart et al.’s model, doctor-patient relationship studies, and patient interviews. It includes 21 items across five subscales: communication and partnership, personal relationship, health promotion, positive approach, and interest in life impact. Using a 4-point Likert scale, the CCM exhibits strong internal consistency across its subscales (Cronbach’s α ranging from .84 to .96). It has been linked to patient satisfaction, enablement, and symptom reduction. The CCM comprehensively assesses all four dimensions of the conceptual framework: disease and illness experience, whole person perspective, common ground, and patient-doctor relationship.
Both the PPPC and CCM are visit-based instruments, making them suitable for assessing patient perceptions of care during individual encounters. While both are valuable tools, the CCM offers a more detailed assessment across multiple subscales and includes the patient-doctor relationship dimension, which is not directly assessed by the PPPC.
Patient-Centered Care Dimensions in Other Instruments
Eleven additional instruments, initially designed for broader healthcare assessments, were found to include relevant subscales or items measuring patient-centered care dimensions. These include the Patient Reactions Assessment (PRA), Perceived Involvement in Care Scale (PICS), Components of Primary Care Instrument (CPCI), Medical Communication Competence Scale (MCCS), Primary Care Assessment Survey (PCAS), Interpersonal Processes of Care (IPC), General Practice Assessment Survey (GPAS), Patient Perception of Quality (PPQ), Primary Care Assessment Tool–Adult Edition (PCAT–A), Consultation and Relational Empathy (CARE), and the Instrument on Doctor-Patient Communication Skills (IDPCS).
These instruments vary in length, focus, and psychometric properties. Notably, instruments like CPCI, PCAS, GPAS, PPQ, PCAT–A, and CARE assess the “whole-person” dimension, while most others cover “common ground,” “disease and illness experience,” and “patient-doctor relationship” to varying degrees. Seven instruments (PRA, CPCI, PCAS, IPC, GPAS, PPQ, and PCAT–A) are designed to assess care over time, offering a broader perspective beyond single visits.
Discussion: Selecting the Right Tool for Measuring Patient Perception
This review highlights the availability of several instruments for measuring patient perception of care in family medicine. For researchers and clinicians specifically seeking to measure patient-centered care, the PPPC and CCM are dedicated and validated options. The choice between these may depend on the specific dimensions of interest and the desired level of detail.
For those interested in a broader assessment of healthcare delivery, instruments like PCAS, GPAS, and PCAT–A offer valuable insights, incorporating patient-centered care as a component within a wider framework. These instruments can be particularly useful for evaluating comprehensive primary care models and system-level changes.
It is important to note that visit-based instruments like PPPC and CCM may have limitations in capturing the longitudinal aspect of patient-centered care, particularly in chronic disease management. The development of longitudinal versions of these instruments could enhance their applicability for assessing care processes over time. Conversely, instruments like PCAT–A, which assess care over a longer period, may be more suitable for evaluating ongoing care experiences.
The increasing emphasis on patient-centered medical homes and healthcare system reforms underscores the growing importance of measuring patient perception of care at both clinical and system levels. While structural and payment reforms are crucial, ensuring that patients perceive their individual needs are at the center of their care remains paramount. Therefore, the selection and application of appropriate measurement tools are essential for driving improvements in patient-centered care delivery.
Further research, including qualitative studies with patients, could refine the conceptual model of patient-centered care and identify the dimensions that are most meaningful to patients and have the greatest impact on long-term outcomes. Additionally, examining the convergent validity of dedicated patient-centered care instruments with subscales from broader healthcare assessment tools would be beneficial.
Limitations
This systematic review acknowledges potential limitations, such as the possibility of omitting relevant articles or unpublished materials despite a comprehensive search strategy. The focus on ambulatory family medicine also means that instruments designed for other healthcare settings were not included. Furthermore, the decision to include instruments measuring at least two dimensions of patient-centered care led to the exclusion of instruments focusing on single dimensions, such as shared decision-making.
Despite these limitations, this review provides a valuable overview of the available tools for measuring patient perception of care in family medicine, offering guidance for clinicians, researchers, and decision-makers seeking to enhance patient-centered practices.
Acknowledgments
The authors express gratitude to Dr. Marie-Dominique Beaulieu, Dr. Moira Stewart, Dr. Paul Little, Dr. Peter Bower, and Dr. Ronald Epstein for their expert contributions and feedback.
Conflicts of interest: authors report none.
Funding support: This research received financial support from the Canadian Health Services Research Foundation (CHSRF).