Section GG is a crucial standardized assessment tool developed by the Centers for Medicare and Medicaid Services (CMS). It’s used across various post-acute care (PAC) settings to evaluate a patient’s functional abilities and assistance needs in self-care and mobility. This assessment also plays a vital role in documenting a patient’s prior level of function. Post-acute care settings where Section GG is utilized include Long-Term Care Hospitals (LTCH), Inpatient Rehabilitation Facilities (IRF), Skilled Nursing Facilities (SNF), and Home Health (HH) agencies.
Accurate scoring of Section GG is not just about patient evaluation; it’s fundamental for reimbursement processes and quality measurement within these healthcare settings. Furthermore, understanding and effectively using Section GG is an excellent way to demonstrate the indispensable value of occupational therapy services in the post-acute care spectrum.
Decoding Section GG in Medicare: What You Need to Know
The Centers for Medicare and Medicaid Services (CMS) leverages Section GG as a standardized method to evaluate patient care and functional status across the continuum of post-acute care. Its significance has grown as it now influences payment and reimbursement models like the Inpatient Rehabilitation Facility Prospective Payment System (IRF PPS) and the Patient-Driven Payment Model (PDPM) in skilled nursing facilities.
The precision in Section GG scoring is paramount. It directly impacts the financial reimbursement facilities receive, which in turn affects their capacity to deliver necessary services to patients. Miscalculations or inaccuracies can lead to underfunding, potentially compromising patient care.
The mandate for standardized outcome measures in post-acute care came from the IMPACT Act of 2014. Prior to Section GG, CMS employed various functional assessments like the Functional Independence Measure (FIM) in inpatient rehab and M1800 items in home health.
However, these earlier tools suffered from inconsistencies. They used different definitions and scoring systems, making it impossible for CMS to effectively track patient progress across different care settings. It was a matter of comparing apples to oranges, hindering consistent evaluation and comparison.
CMS sought a universal language, a standardized assessment, to monitor patient improvement or decline throughout the post-acute care journey. By gathering uniform data through Section GG, CMS can assess the effectiveness and quality of therapy and services provided, drawing conclusions about their impact on patient function and mobility. This standardized approach is what makes Section GG a critical ‘standardized test’ in the realm of post-acute care.
The Link Between Section GG and Reimbursement
CMS recognizes the vulnerability of patients with functional limitations, understanding they face a higher risk of functional decline and mobility-related complications. Section GG serves as a tool to help facilities pinpoint the level and type of services each patient requires.
Moreover, CMS acknowledges the correlation between lower functional levels and increased healthcare utilization. If a patient’s initial assessment overestimates their functional abilities, it can lead to insufficient Medicare reimbursement, failing to cover the full spectrum of services the patient genuinely needs.
Currently, Section GG’s direct influence on reimbursement is primarily within skilled nursing facilities under the Patient-Driven Payment Model (PDPM) and Inpatient Rehabilitation Facilities. However, it’s widely anticipated that its impact will expand to reimbursement models in other post-acute care settings in the future.
Beyond reimbursement, Section GG assessment results are instrumental in guiding clinical decisions. They can trigger necessary interventions to prevent complications related to impaired mobility, such as referrals for occupational therapy or enhanced patient monitoring.
Settings Where Section GG is Mandatory
Section GG is a mandated assessment in the following post-acute care environments:
- Long-Term Care Hospitals (LTCH)
- Inpatient Rehabilitation Facilities (IRF)
- Skilled Nursing Facilities (SNF)
- Home Health (HH)
Ad Break: Support for Content Provided by Medbridge
Medbridge Education is an affiliate link that supports content creation.
Section GG: Measuring Quality Ratings and Patient Outcomes
Section GG is not only about reimbursement; it’s a cornerstone for evaluating outcomes and quality metrics in LTCH, IRF, and SNF settings. While it doesn’t yet directly impact quality outcomes in home health, it remains a mandatory component of the OASIS assessment in that setting. These quality metrics are crucial because they have both direct and indirect effects on reimbursement across all post-acute care settings.
Consistent quality assessment via Section GG provides healthcare agencies with essential feedback for continuous improvement in patient care. These quality measures are publicly accessible on platforms like Care Compare, offering agencies insights into their performance relative to others in their locality. This transparency also empowers patients and facilities to make informed decisions about healthcare providers during recovery.
Ultimately, enhanced quality outcomes can lead to increased patient referrals, thereby boosting revenue for healthcare facilities.
CMS envisions Section GG as a catalyst for better care coordination and discharge planning. The data reported through Section GG informs CMS’s adjustments to payment models. Looking ahead to 2022 and beyond, CMS is implementing quality measures that emphasize the seamless transfer of patient information between different care settings. As value-based purchasing models become more prevalent, quality outcomes will be increasingly linked to reimbursement through incentive bonuses and potential penalties.
Coding and Scoring Section GG: A Detailed Look
Section GG assessments are conducted at a minimum upon admission and discharge in every post-acute care setting. In some cases, it’s also used during reassessments or recertifications. It’s designed as an interdisciplinary assessment, typically completed within the first 3-5 days of admission. Gathering input from various healthcare professionals is crucial for accurately capturing a patient’s functional status.
When scoring Section GG, clinicians should focus on the patient’s typical performance, not their best or worst attempts. The score should represent how the patient performs the activity more than 50% of the time.
It’s important to note that Section GG scoring differs slightly from how occupational therapists might traditionally document self-care and assistance levels. Therefore, CMS training is essential for all clinicians involved in scoring Section GG to ensure data accuracy.
Each Section GG item is scored on a scale of 1 to 6, where 6 indicates complete independence and 1 signifies total dependence. Higher scores reflect greater patient functionality and mobility. Scoring primarily hinges on the level of assistance required, and activities can be performed with or without assistive devices.
Section GG Scoring Definitions: Understanding the Scale
6 – Independent: The patient completes the activity safely on their own without any help.
5 – Setup or Clean-Up Assistance: Helper provides setup or clean-up assistance, but the patient completes the activity independently.
4 – Supervision or Touching Assistance: Helper provides verbal cues, touching, steadying, or contact guard assistance as the patient performs the activity. Assistance can be intermittent or throughout the activity.
3 – Partial/Moderate Assistance: Helper provides less than half the effort. This includes lifting, holding, or supporting limbs or trunk but contributing less than half the effort.
2 – Substantial/Maximal Assistance: Helper provides more than half the effort, including lifting or holding limbs or trunk and contributing more than half the effort.
1 – Dependent: Helper does all the effort. The patient provides no effort to complete the activity, or the activity requires assistance from two or more helpers.
Reasons for Activity Not Attempted (ANA) Codes:
- 07 – Patient/Resident Refused
- 09 – Not Applicable: Activity not attempted and was not performed prior to the current illness, exacerbation, or injury.
- 10 – Not Attempted Due to Environmental Limitations: (e.g., lack of equipment, weather conditions)
- 88 – Not Attempted Due to Medical Condition or Safety Concerns
ANA codes should be used sparingly. In some settings, using an ANA code may default to a score of 1 (dependent) for quality metrics and functional scores. While direct observation is the preferred scoring method, subjective questioning can also be used. Therefore, aim to provide a score between 1-6 whenever possible, resorting to ANA codes only when absolutely necessary.
CMS offers valuable and free Section GG training resources CMS Section GG Training. Clinicians are strongly encouraged to complete this training. CMS also provides helpful video resources for quick reviews.
Observation: The Key to Accurate Section GG Scoring
For the most accurate assessment, observe the patient performing the activity before offering any cues or physical assistance. While CMS allows scoring based on subjective interviews with the patient, family, or hired help, direct observation remains the most reliable method to determine a patient’s true functional status.
During assessment, remember that for a score of 6 (independent), the patient must complete all aspects of the task, including gathering necessary equipment. Providing any form of assistance, even something as seemingly minor as handing shoes or reminding a patient to use bed rails during transfers, would result in a score of 5 or lower, depending on the level of assistance given.
Only provide assistance when it’s essential for safety. Patient safety should always be prioritized over achieving a better Section GG score.
Avoid making assumptions about a patient’s potential functional ability. Scoring based on what you think they could do, rather than what they actually demonstrate, is not beneficial for the patient or the facility.
Ideally, therapeutic interventions and education should commence after Section GG scoring is complete. This doesn’t imply delaying therapy services unnecessarily. Now, let’s explore the three primary sections of Section GG.
Ad Break: Content Support from Medbridge
Medbridge Education is an affiliate link that helps sustain our content.
GG0100. Prior Functioning and GG0110. Prior Device Use: Understanding Patient History
GG0100, Prior Functioning, focuses on the patient’s functional abilities before their current condition. This includes self-care, indoor mobility (ambulation), stair climbing, and functional cognition. Scoring for these items is as follows:
- 3 – Independent: Patient completed activities independently, with or without devices, without helper assistance.
- 2 – Needed Some Help: Patient required partial assistance from another person to complete activities.
- 1 – Dependent: Helper completed activities for the patient.
- 8 – Unknown: Patient’s usual ability prior to the current condition is unknown.
- 9 – Not Applicable: Activity was not applicable to the patient prior to the current condition.
GG0110, Prior Device Use, is collected at admission and records the patient’s prior use of devices, including manual wheelchairs, motorized wheelchairs/scooters, mechanical lifts, walkers, and orthotics/prosthetics. This section uses checkboxes to indicate all applicable devices or “Z” for none of the above.
GG0110. Prior Device Use with Information from Multiple Sources – YouTube
GG0130. Self-Care: Assessing Activities of Daily Living
Self-care items within Section GG are consistent across settings, with a minor variation in LTCH where “bathing” only includes upper body bathing. LTCH does not report on lower body and footwear (F, G, and H). Occupational therapists are uniquely qualified to assess the self-care section due to their expertise in function and activities of daily living.
Key points to remember for self-care items:
- Bathing: Excludes washing hair or back.
- Upper Body Dressing: Includes items like bras, dresses, LTSOs, compression sleeves, abdominal binders, etc. Hospital gowns cannot be used for scoring.
- Lower Body Dressing: Includes donning lower limb prostheses, knee braces, and shrinkers.
- Toileting: Encompasses cleaning and ostomy use but not ostomy bag changes. For patients with indwelling catheters, scoring is based on assistance needed for bowel movements. Toilet transfers are scored separately.
- Footwear: Includes AFOs and compression stockings.
Scoring Showering/Bathing (Section GG 130E)
Consult CMS training materials for detailed guidance.
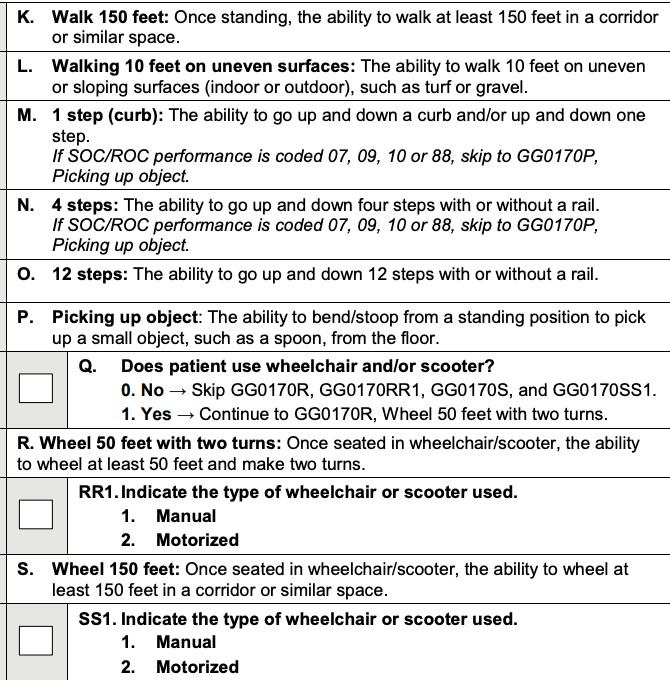
GG0170. Mobility: Evaluating Movement and Transfers
Mobility items are listed below. These are consistent across settings except for minor differences in LTCH. Occupational therapists are well-equipped to score the mobility section. Section GG mobility assessments are not focused on gait patterns or aspects more traditionally associated with physical therapy, though gait assessment remains within the OT scope of practice.
Occupational therapists frequently observe many mobility items during functional assessments. As Section GG is interdisciplinary, gathering data from multiple clinicians ensures a comprehensive and accurate representation of the patient’s typical mobility status.
CMS provides item-specific training for mobility assessments.
Section GG and the Functional Independence Measure (FIM™): Understanding the Relationship
Yes, Section GG effectively replaced the Functional Independence Measure (FIM™) in inpatient rehabilitation facilities (IRF). The FIM™ was not consistently used across all post-acute care settings.
Furthermore, the FIM™ used different scoring methods compared to similar assessments in other settings. Many practitioners also voiced concerns about the FIM™’s sensitivity and the way it grouped certain activities.
Replacing FIM™ with Section GG reduces regulatory burden by eliminating the need for practitioners to score both assessments, streamlining the evaluation process.
Section GG is a standardized assessment implemented by CMS in post-acute care. It assesses a patient’s need for assistance with self-care and mobility, while also documenting their prior functional level. Occupational Therapy expertise is crucial for accurate Section GG scoring.
The Vital Role of Occupational Therapy in Accurate Section GG Scoring
Understanding the interplay between Section GG, reimbursement, and occupational therapy is essential for advocating for occupational therapy involvement early in patient care.
Even if an occupational therapy practitioner isn’t the primary clinician conducting the initial Section GG assessment, they should always share their findings with the reporting clinician. Occupational therapists are the specialists in self-care and functional mobility, making them ideal professionals to contribute to and enhance the accuracy of Section GG assessments in collaboration with other disciplines.
Why Occupational Therapists Are Essential for Section GG Accuracy
Occupational therapy practitioners are inherently generalists with specialized expertise. They excel in task analysis, problem-solving, and comprehensive care planning. All OTs receive extensive training in self-care, activities of daily living (ADLs), instrumental activities of daily living (IADLs), functional cognition, vision, mobility, fall prevention, mental health, and much more.
For a holistic approach to patient care that addresses a wide array of needs, an occupational therapy practitioner is an invaluable asset.
If healthcare employers or organizations are struggling to meet quality benchmarks or consistently face challenges with reimbursement, integrating occupational therapy into the assessment process is a strategic solution.
For OTs working in these settings, proactively engage with managers and use the insights from this article to articulate why occupational therapy is key to resolving these issues. Facility quality scores are publicly available on Care Compare, allowing you to demonstrate how your employer’s performance compares to others in the region.
Occupational Therapy’s Impact on Reimbursement and Patient Outcomes
Accurate Section GG scoring at both evaluation and discharge is crucial for reliable outcome reporting and appropriate revenue generation.
- Overestimating Function at Evaluation:
- Limits the ability to demonstrate patient progress.
- Results in inadequate reimbursement for necessary patient services.
- Negatively impacts quality outcome reporting.
- Underestimating Function at Discharge:
- May falsely indicate functional decline.
- Can make it appear as though a patient hasn’t improved.
- Detrimentally affects quality outcome reporting.
These scenarios are far from ideal and can have significant negative consequences for both revenue and outcome reporting if they occur frequently across patient cases.
Employing and leveraging the expertise of occupational therapists can significantly mitigate these risks. As specialists in assessing self-care and functional mobility, occupational therapists are instrumental in ensuring accurate Section GG scoring, leading to better patient care, appropriate reimbursement, and improved quality outcomes.
Ad Break: Support for Content Provided by Medbridge
Medbridge Education affiliate link supports content creation.
Resources for Further Learning
Ad Break: Content Support from Medbridge