Hand hygiene is paramount in preventing infection transmission, especially in home care settings. This article explores hand hygiene practices among home care nurses, adherence to guidelines, and factors impacting hand hygiene opportunities. We’ll delve into a recent observational study and discuss its implications for improving patient safety in home care.
Observational studies in various healthcare settings consistently reveal suboptimal hand hygiene adherence rates. This issue is particularly critical in home care, where nurses operate with less direct supervision and face unique environmental challenges. A robust hand hygiene audit tool is essential for monitoring and improving practices in this setting.
Assessing Hand Hygiene in Home Care: An Observational Study
A recent study employed the World Health Organization’s “5 Moments for Hand Hygiene” framework, supplemented with three home care-specific opportunities:
- Upon arrival in the home: Addressing potential contamination from external environments.
- Before leaving the patient’s home: Preventing the spread of pathogens to other locations.
- Before accessing the clean compartment of the nursing bag: Maintaining sterility of supplies.
Researchers observed 400 home care visits conducted by 50 nurses, recording a total of 2014 hand hygiene opportunities.
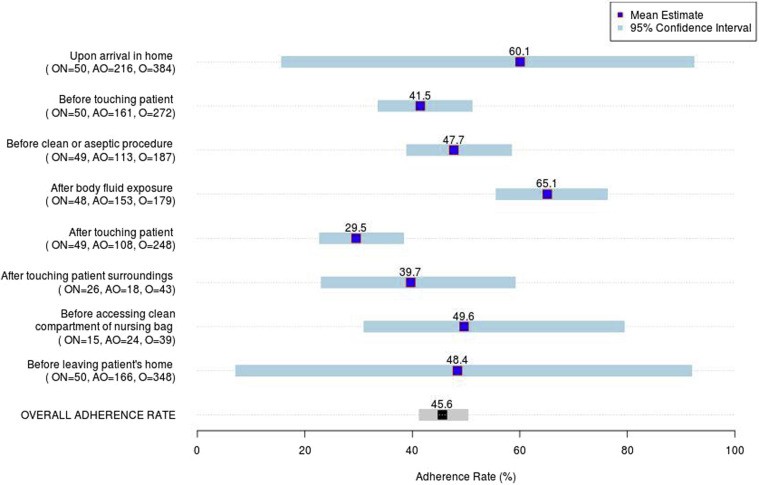 Fig. 1 Nurse-level hand hygiene rate by opportunity
Fig. 1 Nurse-level hand hygiene rate by opportunity
Key Findings and Their Implications
The study revealed an average hand hygiene adherence rate of 45.6% after adjusting for clustering at the nurse level. While adherence was highest after body fluid exposure (65.1%), it was lowest after touching a patient (29.5%).
Surprisingly, nurse demographics and experience did not significantly correlate with adherence rates. However, the study identified crucial environmental factors:
-
Patient infection risk: Higher risk patients presented more hand hygiene opportunities, highlighting the need for targeted interventions. The graphic below illustrates this correlation.
-
Dirty home environment: “Dirty” environments led to increased hand hygiene opportunities, underscoring the importance of patient and caregiver education on environmental cleanliness.
These findings emphasize the necessity of a comprehensive Home Care Hand Hygiene Audit Tool that considers both individual practices and environmental context.
Developing an Effective Home Care Hand Hygiene Audit Tool
Based on the study’s findings, a practical audit tool should incorporate:
- WHO’s 5 Moments: A foundational framework for hand hygiene opportunities.
- Home care-specific moments: Addressing unique challenges in this setting.
- Environmental assessment: Incorporating factors like cleanliness and patient infection risk.
- Observation and feedback: Providing opportunities for improvement through direct observation and constructive feedback.
Conclusion: A Call to Action
This research underscores the urgent need for improved hand hygiene practices in home care. By utilizing a comprehensive home care hand hygiene audit tool that incorporates the WHO framework, home care-specific moments, and environmental assessments, agencies can better monitor adherence, identify areas for improvement, and implement targeted interventions. This proactive approach will significantly reduce infection risk and enhance patient safety in the home care setting. Further research into innovative training methods, such as simulations and case studies, is crucial to address persistent hand hygiene deficiencies.
