Early integration of palliative care (PC) significantly enhances the quality of life for advanced cancer patients. Despite established benefits, PC referrals remain underutilized. This article examines a quality improvement initiative employing a nurse-driven PC referral tool in an outpatient oncology setting to address this gap and answer the question: does a palliative care tool increase palliative referrals?
Identifying the Need for Increased Palliative Care Referrals
Major oncology organizations, including the American Society of Clinical Oncology (ASCO), strongly recommend PC for advanced cancer patients. However, a significant disparity exists between guidelines and actual practice. In a 2018 audit of an outpatient cancer center in Southwestern Pennsylvania, a mere 17.3% of patients with advanced cancer received a PC referral, despite over 94% having distant metastasis. This stark contrast highlighted the urgent need for intervention.
Implementing a Nurse-Driven Palliative Care Referral Tool
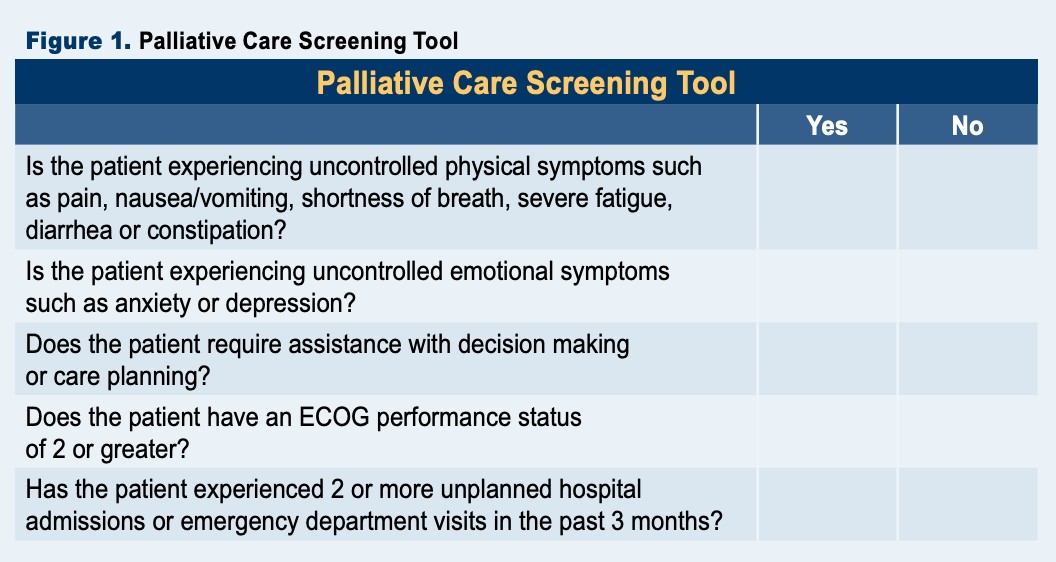
To bridge this gap, a quality improvement project was initiated. The core of this intervention was a three-pronged approach: comprehensive nurse and patient education, a validated PC screening tool, and a formalized nurse-led referral process. Treatment nurses were trained to identify patients not receiving PC and utilize the screening tool (Figure 1). Positive screens triggered patient education and facilitated connections with the cancer center’s PC clinic.
Figure 1. Palliative Care Screening Tool
The screening tool, developed in collaboration with a PC nurse practitioner, comprised five yes/no questions derived from a systematic review and international consensus guidelines. Criteria focused on readily observable factors within the nursing scope of practice. Notably, two criteria, ECOG Performance Status of 2 or greater and two or more hospital/emergency department visits, were validated by local data as predictors of 90-day mortality risk.
Evaluating the Impact of the Palliative Care Tool
The two-month trial demonstrated a substantial increase in PC referrals. The percentage of patients receiving PC jumped from 16.4% to 37.6%. Of 50 eligible patients, 11 (22%) screened positive, leading to PC education for this group. Subsequently, six patients (54.4% of those who screened positive) opted for PC services (Figure 2).
Figure 2. Weekly Palliative Care Utilization
Beyond the statistical improvement, the initiative garnered positive feedback from both nurses and patients. Nurses reported increased confidence in discussing PC and found the referral process rewarding. Patients expressed appreciation for learning about available resources, with one noting significant relief from suffering after engaging with PC.
Sustaining and Expanding the Initiative: Answering the Question
The success of the trial led to the permanent adoption of the PC screening tool and procedures within the unit and its integration into the electronic medical record. Plans are underway to expand implementation across the cancer center. This initiative demonstrates that a structured approach, utilizing a practical screening tool and empowering nurses, can significantly increase PC referrals. Therefore, in answer to the question “Does A Palliative Care Tool Increase Palliative Referals?”, the evidence suggests a resounding yes.
References
- Temel JS, et al. Am J Clin Oncol. 2017;35(8):834-841.
- Vanbutsele G, et al. Lancet Oncol. 2018;19(3):394-404.
- Zhuang H, et al. Curr Oncol. 2018;25(1):54-58.
- Zimmermann C, et al. Lancet Oncol. 2014;383(9930):1721-1730.
- Bakitas MA, et al. Am J Clin Oncol. 2015;33(13):1438-1445.
- King JD, et al. J. Pain and Symptom Manage. 2016;51(6):1027-1032.
- Institute of Medicine of the National Academies. Dying in America: Improving Quality and Honoring Individual Preferences Near the End of Life. 2015.
- Ferrell BR, et al. Am J Clin Oncol. 2017;35(1):96-112.
- National Comprehensive Cancer Network. Palliative Care (Version 2.2021).
- Goldwasser F, et al. Cancer. 2018;124(14):3044-3051.
- Michael N, et al. BMC Palliat Care. 2019;18(1).
- Osagiede O, et al. J Palliat Care. 2018;33(3):149-158.
- Hui D, et al. Oncologist. 2016;21(7):895-901.
- Hui D, et al. Lancet Oncol. 2016;17(12):552-559.