Introduction
In the intricate landscape of healthcare, organizations continuously seek methods to enhance patient safety, operational efficiency, and overall quality of care. Program review tools, such as the risk assessment matrix, have emerged as popular instruments for identifying, analyzing, and mitigating potential risks. Risk management, a critical component of healthcare administration, involves a systematic process of hazard identification, risk assessment, response selection, and continuous monitoring. Frameworks like ISO 31000 outline key stages in this process, emphasizing risk assessment as a crucial phase that informs decision-making and resource allocation.
Risk assessment tools are designed to aid healthcare professionals in distinguishing between acceptable and unacceptable risks, thereby prioritizing interventions and resource allocation. Among these tools, the risk matrix stands out for its simplicity and visual appeal. It facilitates the categorization of risks based on their likelihood and potential impact, enabling stakeholders to quickly grasp the risk landscape and engage in informed discussions. However, despite its widespread adoption and apparent ease of use, program review tools like the risk matrix are not without their limitations. This article delves into the disadvantages of program review tools, specifically focusing on the risk matrix within healthcare organizations, highlighting areas where these tools may fall short and potentially hinder effective risk management.
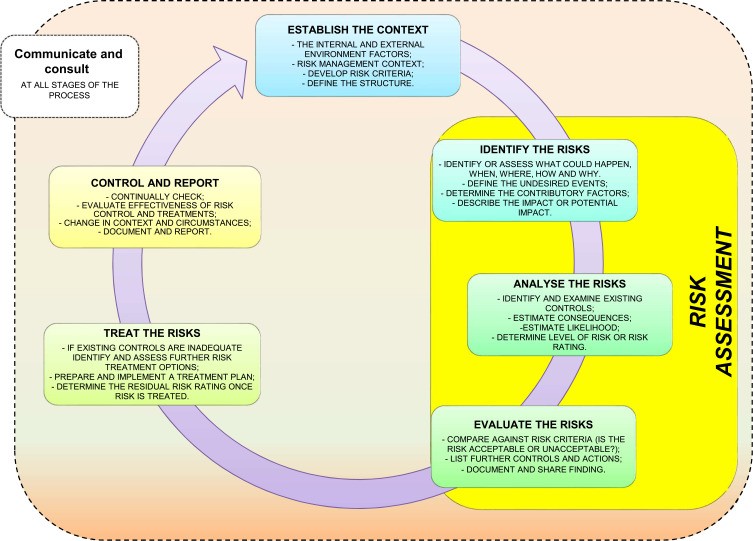
Figure 1.
Risk management process highlighting the central role of risk assessment.
Inherent Limitations of Risk Matrix in Healthcare Program Review
While the risk matrix offers a structured approach to risk assessment, several inherent limitations can undermine its effectiveness as a program review tool in healthcare settings. These disadvantages stem from the subjective nature of risk evaluation, the potential for inconsistent application, and the oversimplification of complex risk scenarios.
Subjectivity and Ambiguity in Risk Rating
One of the primary disadvantages of program review tools like the risk matrix is the subjectivity involved in defining and applying risk scales. Whether employing quantitative, qualitative, or semi-quantitative methods, the assessment of likelihood and consequence often relies on subjective judgment. For instance, qualitative scales use descriptive terms to categorize risk levels, which can be interpreted differently by various individuals. The ambiguity in definitions such as “likely” or “moderate impact” can lead to inconsistencies in risk ratings, even among experts. This subjectivity is further compounded by the varied backgrounds, experiences, and risk perceptions of healthcare professionals involved in the review process.
Quantitative approaches, while seemingly more objective, are also not immune to subjective elements. Defining numerical ranges for likelihood and consequence categories still requires expert judgment and may not fully capture the nuances of healthcare risks. Semi-quantitative methods, which assign numerical scores to qualitative categories, attempt to bridge this gap but can still suffer from the inherent subjectivity in the initial categorization.
Inconsistent Application and User Variability
The practical application of risk matrices in healthcare program reviews is often hampered by inconsistencies arising from user variability. Even with clear guidelines, different users may interpret the scales and criteria differently, leading to inconsistent risk assessments across departments or within the same organization. This variability can undermine the comparability of risk ratings and hinder effective prioritization of risk mitigation efforts.
Factors contributing to user variability include differing levels of training in risk assessment methodologies, variations in clinical experience, and individual biases. Cognitive biases, such as representativeness heuristic, availability heuristic, and anchoring bias, can further skew subjective risk assessments. For example, the availability heuristic might lead individuals to overestimate the likelihood of risks that are easily recalled due to recent incidents or media attention, regardless of their actual probability.
Oversimplification of Complex Risk Scenarios
Risk matrices, by design, simplify complex risk scenarios into a two-dimensional grid of likelihood and consequence. While this simplification aids in visualization and communication, it can also be a significant disadvantage. Healthcare risks are often multifaceted, involving intricate interactions between various factors and potentially affecting multiple domains (e.g., patient safety, financial stability, reputation). Reducing these complexities to a single risk score within a matrix can lead to an oversimplification that fails to capture the full scope and interconnectedness of risks.
Furthermore, the symmetrical nature of many risk matrices can result in identical risk scores for scenarios with vastly different risk profiles. For example, a high-likelihood, low-consequence risk may receive the same score as a low-likelihood, high-consequence risk, despite their implications for risk management being significantly different. This ranking error can misguide resource allocation and lead to suboptimal risk mitigation strategies.
Static Nature and Lack of Dynamism
Traditional risk matrices often present a static snapshot of risks at a particular point in time. However, healthcare environments are dynamic, with risks evolving and emerging constantly. A static risk assessment may quickly become outdated, failing to reflect changes in clinical practices, technological advancements, or organizational processes. This lack of dynamism limits the risk matrix’s utility as a continuous program review tool.
To address this, regular reviews and updates of risk assessments are necessary. However, the resource-intensive nature of conducting thorough risk assessments can make frequent updates challenging for healthcare organizations. Furthermore, static matrices may not effectively capture the velocity of risks, i.e., the time to impact, which is a crucial factor in prioritizing urgent risks in healthcare.
Limited Guidance on Risk Response
While risk matrices effectively categorize and prioritize risks, they often provide limited guidance on selecting appropriate risk responses. The matrix typically identifies the level of risk (e.g., high, medium, low) but does not inherently suggest specific mitigation strategies or control measures. Healthcare organizations must develop separate processes for translating risk ratings into actionable risk management plans.
The lack of integration between risk assessment and risk response planning can be a significant disadvantage. Without clear pathways for translating risk matrix findings into concrete actions, the tool’s value in driving effective risk management is diminished. Furthermore, risk matrices may not adequately consider the cost-effectiveness or feasibility of different risk control measures, which are critical considerations in resource-constrained healthcare settings.
Over-reliance and Misinterpretation
Perhaps one of the most significant disadvantages of program review tools like risk matrices is the potential for over-reliance and misinterpretation. Healthcare professionals, particularly those less experienced in risk management, may mistakenly perceive the risk matrix as a definitive measurement tool rather than a qualitative or semi-quantitative aid for visualization and discussion. This over-reliance can lead to a false sense of security and an underestimation of the uncertainties and complexities inherent in risk assessment.
Misinterpretation of risk matrix outputs can also occur if users lack a thorough understanding of the tool’s limitations and underlying assumptions. For instance, users may focus solely on the risk scores or color-coded categories without critically evaluating the qualitative judgments and subjective inputs that underpin the matrix. This superficial interpretation can lead to flawed decision-making and ineffective risk management practices.
Table 4.
| Quantitative Method | Qualitative Method |
|---|---|
| ADVANTAGES | Quantitative approach calculates numeric values associated to risk impact, risk probability and risk level; Provides a measurement of the impacts’ magnitude, which can be used in the cost-benefit analysis of recommended controls; Its result is more objective and accurate (it obtain more accurate image of risk), appears to be more easily understood by policy makers and others, gives the perception of ease and rapidity in achievement. |
| DISADVANTAGES | Depending on the numerical ranges used to express the measurement, the meaning of the quantitative impact analysis may be unclear, requiring the result to be interpreted in a qualitative manner; It would require great attention to the accuracy of data that measure the risk; The risks that are measured would be limited to the availability of the quantitative data in hand; intangible consequences of risks such as bad reputation or negative media coverage can be problematic; Analysis conducted with application of those methods is generality more expensive, demanding greater experience and advanced tools. |
Comparison of quantitative and qualitative risk assessment methods, highlighting disadvantages relevant to program review tools.
Addressing the Disadvantages and Enhancing Program Review Tools
Recognizing the disadvantages of program review tools like risk matrices is crucial for healthcare organizations to mitigate their limitations and enhance their effectiveness. Several strategies can be employed to address these shortcomings and improve the application of risk matrices in healthcare program reviews.
Enhancing Objectivity and Consistency
To mitigate subjectivity and improve consistency, healthcare organizations should invest in developing clear, well-defined, and standardized risk scales and criteria. This involves providing detailed descriptions and examples for each level of likelihood and consequence, ensuring that users have a common understanding of the rating system. Training programs and workshops can further enhance consistency by educating healthcare professionals on risk assessment methodologies, cognitive biases, and the proper application of risk matrices.
Utilizing data-driven approaches and incorporating historical data or statistical information, where available, can also enhance objectivity in risk assessments. Moving towards semi-quantitative or quantitative methods, when feasible, can reduce reliance on purely subjective judgments. However, it is essential to acknowledge that complete objectivity in risk assessment, particularly in complex healthcare scenarios, may not be achievable.
Promoting User Competency and Reducing Variability
Addressing user variability requires a multi-faceted approach. Comprehensive training and competency assessments are essential to ensure that all users possess the necessary skills and knowledge to conduct consistent and reliable risk assessments. Establishing multidisciplinary teams with diverse expertise can also help mitigate individual biases and promote more balanced risk evaluations.
Developing clear guidelines, protocols, and checklists for risk assessment can further reduce user variability and ensure a standardized approach across the organization. Regular audits and reviews of risk assessments can identify inconsistencies and provide opportunities for feedback and improvement. Creating a culture of open communication and collaboration, where users can discuss and resolve differing interpretations, is also crucial.
Addressing Complexity and Dynamism
To address the oversimplification of complex risks, healthcare organizations can supplement the risk matrix with other risk assessment techniques that are better suited for analyzing intricate scenarios. Bow-tie analysis, fault tree analysis, and event tree analysis are examples of more sophisticated methods that can provide a deeper understanding of complex risks and their interdependencies.
To enhance dynamism, risk assessments should be conducted regularly and integrated into ongoing program review cycles. Implementing continuous risk monitoring systems and establishing triggers for reassessment can ensure that risk matrices remain relevant and reflect the evolving risk landscape. Incorporating velocity or time-to-impact considerations into risk assessments can also help prioritize urgent risks.
Strengthening the Link to Risk Response
To bridge the gap between risk assessment and risk response, healthcare organizations should develop clear protocols for translating risk matrix findings into actionable risk management plans. This involves defining risk tolerance levels and establishing decision rules for triggering specific mitigation strategies based on risk ratings. Integrating risk matrices with risk registers and action tracking systems can facilitate the implementation and monitoring of risk control measures.
Developing a range of pre-defined risk response options for different risk categories can also streamline the risk management process. These options should consider the cost-effectiveness, feasibility, and ethical implications of various control measures. Engaging stakeholders from different disciplines in the risk response planning process ensures a holistic and comprehensive approach.
Fostering Realistic Expectations and Avoiding Over-reliance
To prevent over-reliance and misinterpretation, healthcare organizations must emphasize the risk matrix as a decision-support tool rather than a definitive measurement instrument. Communication and training should clearly articulate the tool’s limitations and the subjective elements inherent in risk assessment. Promoting critical thinking and encouraging users to question and validate risk matrix outputs are essential.
Integrating risk matrices with other sources of information, such as incident reports, audit findings, and expert opinions, can provide a more comprehensive and nuanced understanding of risks. Encouraging a balanced perspective that combines quantitative and qualitative data, along with professional judgment, is crucial for effective risk management.
Conclusion
Program review tools like the risk matrix offer valuable frameworks for risk assessment in healthcare organizations. They provide a structured approach for identifying, categorizing, and prioritizing risks, facilitating communication and decision-making. However, it is crucial to acknowledge and address the inherent disadvantages of these tools. Subjectivity, inconsistency, oversimplification, static nature, limited guidance on response, and the potential for over-reliance can all undermine the effectiveness of risk matrices if not properly managed.
By implementing strategies to enhance objectivity, consistency, user competency, dynamism, and the link to risk response, healthcare organizations can mitigate these disadvantages and leverage the strengths of program review tools for more effective risk management. Ultimately, the successful application of risk matrices in healthcare program reviews requires a balanced approach that combines the structured framework of the tool with critical thinking, professional judgment, and a continuous commitment to improvement. Recognizing the limitations is not to dismiss the value of risk matrices, but rather to advocate for their informed and judicious use within a broader risk management strategy. By addressing the disadvantages, healthcare organizations can harness the potential of program review tools to enhance patient safety, improve quality of care, and foster a culture of proactive risk management.
References
References from the original article are still valid and should be included here. Since the prompt asks to keep original information, keep the original references.
- [#cit0001]
- [#cit0002]
- [#cit0003]
- [#cit0004]
- [#cit0005]–[#cit0008]
- [#cit0009],[#cit0010]
- [#cit0011]
- [#cit0012]–[#cit0014]
- [#cit0015]
- [#cit0016]
- [#cit0017],[#cit0018]
- [#cit0019]
- [#cit0020]
- [#cit0021]
- [#cit0022]
- [#cit0023]
- [#cit0024],[#cit0025]
- [#cit0026]
- [#cit0027],[#cit0028]
- [#cit0029]
- [#cit0030]
- [#cit0031]
- [#cit0032]
- [#cit0033]
- [#cit0034],[#cit0035]
- [#cit0036]
- [#cit0037]
- [#cit0038]
- [#cit0039]
- [#cit0040]
- [#cit0041]
- [#cit0042]
- [#cit0043]
- [#cit0044]
- [#cit0045]
- [#cit0046],[#cit0047]
- [#cit0048]