Introduction
Pain assessment in patients within the Intensive Care Unit (ICU) presents a significant challenge for healthcare professionals. Patients in the ICU are often unable to self-report pain due to intubation, sedation, or altered levels of consciousness. This inability to communicate necessitates the use of objective pain assessment tools to ensure patient comfort and effective pain management. Among these tools, the Critical Care Pain Observation Tool (CPOT) stands out as a validated and reliable method for evaluating pain in non-communicating, critically ill adults. Understanding and utilizing the CPOT is crucial for healthcare providers aiming to deliver optimal care and improve patient outcomes in the critical care setting. This article delves into the CPOT, exploring its development, validation, and practical application in pain management for intubated patients.
Critically ill patients are routinely subjected to numerous painful procedures and experience pain from their underlying conditions. Studies indicate that a substantial proportion of ICU patients report significant pain, both at rest and during routine nursing procedures. Inadequate pain assessment can lead to undertreatment of pain, which can negatively impact patient recovery, prolong mechanical ventilation, and extend ICU stays. Therefore, accurate and consistent pain assessment using tools like the CPOT is not just a matter of patient comfort, but a critical component of quality care in the ICU.
Recognizing pain management as a fundamental patient right and a professional duty, healthcare providers must be adept at utilizing validated pain assessment scales when self-reporting is not possible. The CPOT, alongside tools like the Behavioral Pain Scale (BPS), provides a structured and objective approach to pain assessment. These behavioral scales focus on observable indicators such as facial expression, body movements, muscle tension, and ventilator compliance (or vocalization in extubated patients). The CPOT, specifically designed for critically ill patients, offers a practical and effective way to monitor and manage pain in those unable to articulate their discomfort. This review aims to provide a comprehensive understanding of the CPOT, its validation, and its role in enhancing pain management in intubated ICU patients.
Table 1: Behavioral Pain Scale
| Indicator | Item | Score |
|---|---|---|
| Facial expression | Relaxed | 1 |
| Partially tightened = brow lowering | 2 | |
| Fully tightened = eyelid closing | 3 | |
| Grimacing | 4 | |
| Upper limb | No movement | 1 |
| Partially bent | 2 | |
| Fully bent with finger flexion | 3 | |
| Permanently retracted | 4 | |
| Compliance with ventilation | Tolerating movement | 1 |
| Coughing but tolerating ventilation most of the time | 2 | |
| Fighting ventilator | 3 | |
| Unable to control ventilation | 4 | |
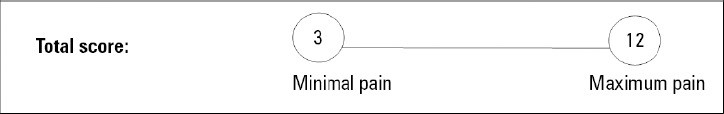
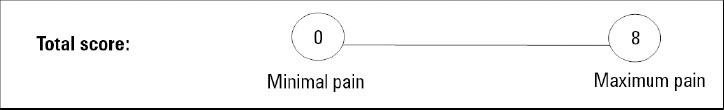
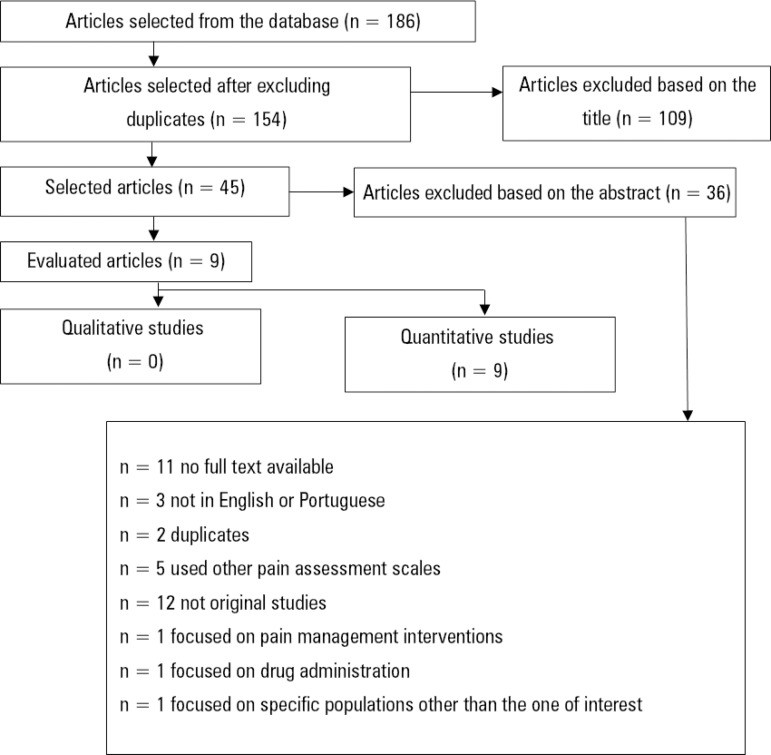
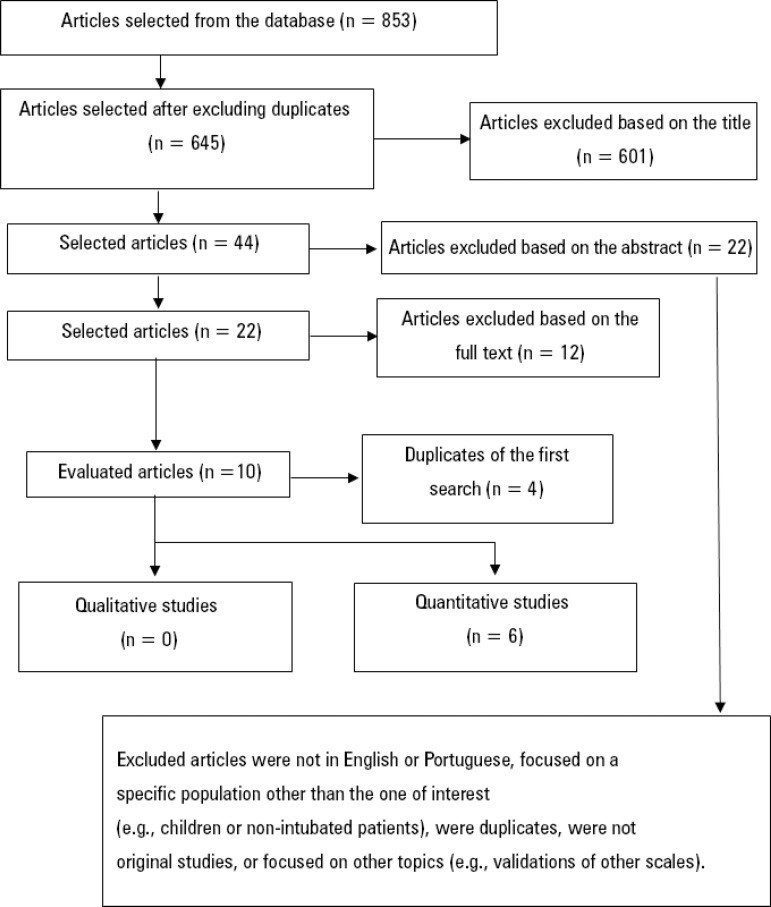
Table 2: Critical Care Pain Observation Tool
| Indicator | Item | Score |
|---|---|---|
| Facial expression | Relaxed | 0 |
| Tense | 1 | |
| Grimacing | 2 | |
| Body movements | Absence of movements | 0 |
| Protection | 1 | |
| Restlessness | 2 | |
| Muscle tension | Relaxed | 0 |
| Tense or rigid | 1 | |
| Very tense or rigid | 2 | |
| Compliance with the ventilator (intubated patients)/vocalization (extubated patients) | Tolerating ventilator or movement/talking in a normal tone or no sound | 0 |
| Coughing but tolerating ventilator/sighing, moaning | 1 | |
| Fighting ventilator/crying out, sobbing | 2 | |
Methods: Systematic Review Approach
This article is based on a systematic literature review, adhering to the rigorous methodology recommended by the Cochrane Center. This approach ensures a comprehensive and unbiased analysis of existing research on the effectiveness of pain assessment scales in the ICU setting. The review specifically focused on the Behavioral Pain Scale (BPS) and the Critical Care Pain Observation Tool (CPOT) and their suitability for assessing pain in adult patients who are orotracheally intubated and admitted to the ICU.
The review employed a structured search strategy within the EBSCO Host database, encompassing CINAHL Complete, MEDLINE® Complete, Nursing & Allied Health Collection: Comprehensive, Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, Cochrane Methodology Register, Library, Information Science & Technology Abstracts, and MedicLatina. Two independent searches were conducted using the terms “behavioral pain scale” AND “critical care pain observation tool” and “behavioral pain scale” OR “critical care pain observation tool”. This dual search strategy aimed to capture a broad spectrum of relevant studies.
Study selection was based on predefined PICo criteria: Participants (adult inpatients over 18 years), Point of Interest (BPS and CPOT pain assessment scales), and Context (ICU setting). Exclusion criteria were applied to filter out studies focused on pediatric populations, non-ICU settings, other pain scales, qualitative research, and non-original studies. Studies directly comparing BPS and CPOT or highlighting the individual advantages of each scale were prioritized for inclusion.
The methodological quality of the selected studies was rigorously assessed by two independent reviewers using instruments from the Joanna Briggs Institute (MAStARI), specifically the MAStARI Checklist for Diagnostic Test Accuracy Studies. Only studies demonstrating high methodological quality, defined as a score of 8 to 10 on the MAStARI checklist, were included in the final synthesis. This rigorous selection process ensures that the conclusions drawn in this review are based on robust and reliable evidence.
Results: Validation and Reliability of CPOT
The systematic review identified fifteen high-quality studies that evaluated the Behavioral Pain Scale (BPS) and the Critical Care Pain Observation Tool (CPOT) for pain assessment in orotracheally intubated patients within the intensive care unit. These studies consistently demonstrated that both the BPS and CPOT are valid and reliable tools for this purpose. The research spanned various countries and healthcare settings, reinforcing the generalizability of these findings.
The validation studies assessed several key psychometric properties of both scales, including interrater reliability, internal consistency, and criterion validity. Interrater reliability, which measures the consistency between different observers using the same scale, was consistently good for both CPOT and BPS across the studies. This indicates that different healthcare professionals can use these tools and arrive at similar pain assessments, enhancing the objectivity and consistency of pain management.
Internal consistency, reflecting how well the different items within each scale measure the same construct, was also found to be adequate for both scales. Criterion validity, which assesses how well the scales correlate with other measures of pain or pain-related behaviors, was supported by findings that CPOT and BPS scores increased significantly during painful procedures compared to periods of rest. This responsiveness to pain stimuli further validates their use in clinical practice.
While both scales demonstrated strong psychometric properties overall, some studies highlighted nuances. For instance, one study noted that while most indicators in both scales increased during painful procedures, only BPS indicators increased during non-painful procedures, suggesting potential differences in discriminant validity. However, the general consensus across the reviewed literature is that both CPOT and BPS are valuable tools for pain assessment in intubated ICU patients, exhibiting comparable reliability and validity. The validation of CPOT across various languages and cultural contexts, including Swedish, Brazilian Portuguese, Danish, and Icelandic versions, further underscores its broad applicability.
Figure 1: Flow chart of the included studies – first search.
Figure 2: Flow chart of the included studies – second search.
Discussion: CPOT in Clinical Practice
The findings of this systematic review reinforce the importance of utilizing objective pain assessment tools like the Critical Care Pain Observation Tool (CPOT) and the Behavioral Pain Scale (BPS) in the ICU, particularly for patients unable to self-report pain. Both scales have demonstrated robust psychometric properties, making them valuable assets in pain management. The CPOT and BPS provide healthcare professionals with structured methods to identify and quantify pain based on observable behaviors, leading to more effective pain management strategies.
While both scales are effective, there are subtle differences that may influence clinical preference. The BPS, with its domain specifically addressing compliance with ventilation, is particularly well-suited for patients undergoing invasive mechanical ventilation. Conversely, the CPOT offers broader applicability by including a vocalization domain, making it suitable for both intubated and extubated patients. This versatility can be advantageous in dynamic ICU settings where patients may transition between intubated and extubated states.
Some studies suggest that the BPS may be slightly more feasible and easier to remember for clinicians, while others highlight the CPOT’s stronger discriminant validity, noting that CPOT scores are less likely to be influenced by non-painful stimuli. Ultimately, the choice between CPOT and BPS may depend on the specific clinical context and patient population. Some researchers even propose the simultaneous use of both scales to potentially enhance pain detection and assessment accuracy.
A consistent finding across the reviewed studies is the sensitivity of both CPOT and BPS to painful procedures. Both scales demonstrated significant increases in scores during painful interventions, reflecting their ability to detect procedural pain. Key indicators that showed notable changes during painful procedures include facial expression in the BPS and muscle tension, facial tension, and ventilator tolerance/cough in the CPOT. These findings underscore the clinical utility of these scales for monitoring pain responses to routine procedures in the ICU.
Furthermore, correlations between pain scores and vital signs, particularly blood pressure, have been observed. While elevated blood pressure can be indicative of pain, it is not a specific or reliable sole indicator. Therefore, relying solely on vital signs for pain assessment is insufficient, and tools like CPOT provide a more direct and behaviorally-grounded approach.
Despite their overall effectiveness, limitations of both CPOT and BPS have been noted in specific patient populations. Patients with neurological injuries, traumatic brain injury, or burns may present unique challenges for behavioral pain assessment. In these populations, some indicators of pain may be altered or masked by the underlying condition. Further research is warranted to refine pain assessment strategies in these complex patient groups.
Practical considerations for implementing CPOT and BPS in the ICU are largely positive. Healthcare professionals generally find both scales easy to use and remember, facilitating their integration into routine care. The use of these scales has been associated with increased frequency of pain assessments and potentially a more judicious use of analgesics and sedatives, aligning with best practices for pain management and minimizing unnecessary medication exposure.
Conclusion: Enhancing Pain Management with CPOT
This systematic review confirms the Critical Care Pain Observation Tool (CPOT) and the Behavioral Pain Scale (BPS) as valid and reliable instruments for pain assessment in orotracheally intubated, critically ill patients across diverse cultural settings. Both tools effectively detect pain responses during painful procedures, primarily through indicators such as facial expressions (BPS) and muscle tension/ventilator compliance (CPOT), along with changes in blood pressure.
While some debate exists regarding the optimal scale and their application across varying levels of consciousness and sedation, the evidence strongly supports the use of at least one of these scales in routine ICU practice. Implementing CPOT or BPS can lead to more frequent and systematic pain assessments, potentially optimizing analgesic and sedative administration and improving overall patient care.
Moving forward, further research is encouraged to explore the application of CPOT and BPS in specific critically ill populations, including trauma, burn, and neurosurgical patients. Investigating the optimal integration of these scales into comprehensive pain management protocols and evaluating their impact on patient outcomes remain important areas for future study. For now, the CPOT stands as a valuable tool for healthcare professionals striving to provide effective pain management for their most vulnerable patients in the intensive care unit.
References
(References are kept the same as the original article)
