Introduction
In the demanding world of healthcare, nurses and midwives stand as pillars of strength and compassion. They are the frontline caregivers, dedicating themselves to the well-being of others. However, the very nature of their profession, characterized by long hours, emotional strain, and high-pressure environments, often places their own health and well-being at risk. The World Health Organization emphasizes self-care as a fundamental aspect of health for everyone, including healthcare professionals, defining it as the ability to promote health, prevent disease, and manage illness, with or without professional support [1]. For nurses, self-care is not a luxury but a necessity, crucial for sustaining their ability to provide quality patient care and for safeguarding their personal health.
The concept of self-care for nurses isn’t new. Dorothea E. Orem’s self-care deficit theory, introduced in 1956, initially focused on patient self-care. However, it implicitly highlighted the need for caregivers to also engage in self-care to effectively support their patients [3]. Today, self-care for nurses has evolved to encompass a holistic approach, recognizing seven key components: health maintenance and promotion, illness management, fostering self-reliance, addressing diverse populations, promoting personal responsibility, involving healthcare professionals collaboratively, and integrating within the broader health system [4].
In today’s healthcare landscape, especially in the wake of global health crises like the COVID-19 pandemic, the importance of nurse self-care is amplified. The pandemic has placed unprecedented pressure on healthcare systems and professionals, leading to increased stress, burnout, and mental health challenges [7,8]. Recognizing and addressing these challenges requires a proactive approach, starting with self-awareness and assessment. This is where self-care assessment tools become invaluable for nurses.
This article delves into the critical role of self-care assessment tools for nurses. We will explore the core concepts underpinning self-care – mindfulness, compassion, and resilience – and how these are integral to a nurse’s well-being. Furthermore, we will examine the types of self-care assessment tools available, their benefits, and how they can be effectively implemented to foster a culture of self-care within nursing practice. By understanding and utilizing these tools, nurses can take the first crucial step towards prioritizing their own well-being, ultimately enhancing both their personal and professional lives.
Understanding Self-Care Concepts: Mindfulness, Compassion, and Resilience
The concept of self-care for nurses is deeply intertwined with three key constructs: mindfulness, compassion, and resilience. These are not isolated traits, but rather interconnected elements that contribute to a nurse’s overall well-being and ability to provide effective care.
Mindfulness: Being Present in the Moment
Mindfulness, as a self-care practice, is about cultivating present moment awareness without judgment [25]. For nurses, mindfulness can be particularly beneficial in managing the emotional demands of their profession. It involves:
- Awareness of Thoughts and Feelings: Recognizing and acknowledging negative thoughts and emotions without being overwhelmed by them [23].
- Present Moment Focus: Paying attention to the present experience, allowing nurses to detach from rumination about the past or anxiety about the future [22].
- Balanced Response: Facilitating a more thoughtful and flexible reaction to stressful situations, rather than an automatic or reactive response [30].
Self-awareness is closely linked to mindfulness, representing a conscious understanding of one’s own reactions and emotional states [33]. Dispositional mindfulness, or the innate ability to “be mindful,” is also recognized as a protective factor against stress in both personal and professional life [27,29].
Compassion: Caring for Self and Others
Compassion is the ability to recognize and empathize with suffering, coupled with a desire to alleviate it [33]. In nursing, compassion extends in two directions: towards patients and towards oneself. Key aspects of compassion include:
- Kindness: Basic kindness and understanding towards oneself and others in moments of difficulty [23].
- Shared Humanity: Recognizing that suffering is a universal human experience, fostering connection rather than isolation [23].
- Empathy: Understanding and sharing the feelings of others, particularly patients in distress [24].
Self-compassion is particularly vital for nurses. It involves directing compassion inward, treating oneself with the same kindness and understanding one would offer to a patient or colleague [28]. Self-compassion is composed of self-kindness, recognizing common humanity, and mindfulness [23]. It allows nurses to acknowledge their own suffering without self-criticism, fostering emotional resilience [23].
Compassion satisfaction refers to the positive feelings and fulfillment derived from caregiving, representing the rewarding aspects of a nurse’s professional life [20,22]. This satisfaction is crucial for maintaining well-being and coping resources [22]. Conversely, compassion fatigue is a state of emotional and physical exhaustion caused by prolonged exposure to suffering [24]. It is characterized by a reduced capacity for empathy and can lead to burnout and secondary traumatic stress [22].
Resilience: Bouncing Back from Adversity
Resilience is the ability to adapt well in the face of adversity, trauma, tragedy, threats, or significant sources of stress [30]. It is not simply bouncing back to a previous state, but also involves personal growth and transformation through challenging experiences [21]. Resilience is not a fixed trait, but rather a set of skills and behaviors that can be learned and strengthened [30]. Key components of resilience include:
- Self-efficacy: Belief in one’s ability to succeed in specific situations or accomplish a task [26].
- Coping Mechanisms: Effective strategies for managing stress and challenges.
- Adaptability: Flexibility and willingness to adjust to changing circumstances.
- Social Support: Strong connections with colleagues, friends, and family.
Strategies to foster resilience in nurses include promoting social connections, encouraging positivity, leveraging strengths, nurturing growth, supporting self-care practices, fostering mindfulness, and conveying altruism [31].
The Interconnection: Building a Foundation for Self-Care Assessment
Mindfulness, compassion, and resilience are not isolated concepts; they are interconnected and mutually reinforcing. Mindfulness enhances self-awareness, which is foundational for self-compassion and building resilience. Self-compassion buffers against the negative impacts of stress and fosters emotional resilience. Resilience, in turn, supports the sustained practice of mindfulness and compassion, creating a positive cycle of well-being.
Understanding these interconnected concepts is crucial for effectively utilizing self-care assessment tools. These tools are designed to evaluate a nurse’s standing in these key areas, providing insights into their current well-being and highlighting areas where self-care practices can be strengthened. By assessing mindfulness, compassion, and resilience, nurses can gain a clearer picture of their self-care needs and take proactive steps towards enhancing their overall health and professional effectiveness.
The Vital Role of Self-Care Assessment Tools for Nurses
Self-care assessment tools are structured questionnaires or inventories designed to evaluate various aspects of an individual’s self-care practices and well-being. For nurses, these tools serve as a critical starting point for prioritizing their health and professional longevity. They play a vital role in several key areas:
Early Identification of Burnout and Compassion Fatigue
One of the primary benefits of self-care assessment tools is their ability to detect early warning signs of burnout and compassion fatigue. These conditions can develop gradually, often unnoticed until they significantly impact a nurse’s physical and mental health, as well as their job performance. Regular self-assessments can help nurses:
- Recognize Symptoms: Identify symptoms like emotional exhaustion, cynicism, reduced personal accomplishment (burnout), and secondary traumatic stress (compassion fatigue) early on.
- Track Changes Over Time: Monitor their well-being trends, noticing when stress levels are rising or self-care practices are slipping.
- Proactive Intervention: Enable timely interventions to address these issues before they escalate into more serious problems.
Promoting Proactive Self-Care Strategies
Assessment tools are not just diagnostic; they are also catalysts for action. By highlighting areas where self-care is lacking, these tools empower nurses to:
- Increase Self-Awareness: Gain a deeper understanding of their personal self-care needs and habits.
- Identify Areas for Improvement: Pinpoint specific areas where they can enhance their self-care practices, such as mindfulness, stress management, or work-life balance.
- Develop Personalized Plans: Inform the development of tailored self-care plans that address their unique needs and challenges.
Enhancing Nurse Well-being and Retention
Investing in nurse well-being is not only ethically sound but also strategically important for healthcare organizations. Self-care assessment tools contribute to a healthier and more supportive work environment, leading to:
- Improved Mental and Physical Health: Promoting proactive self-care reduces stress, improves mental health, and enhances overall physical well-being.
- Increased Job Satisfaction: Nurses who feel supported and are equipped to care for themselves tend to experience higher job satisfaction.
- Reduced Turnover Rates: Addressing burnout and promoting well-being can significantly reduce nurse turnover, saving organizations recruitment and training costs, and ensuring continuity of care.
Improving Patient Care Quality
Ultimately, nurse self-care directly impacts the quality of patient care. Nurses who are well-rested, emotionally balanced, and resilient are better equipped to provide compassionate and effective care. Self-care assessment tools contribute to improved patient care by:
- Enhancing Empathy and Compassion: Nurses who practice self-compassion are better able to extend compassion to their patients.
- Reducing Errors: Burnout and fatigue can increase the risk of medical errors. Prioritizing self-care helps nurses maintain focus and alertness.
- Creating a Positive Care Environment: A nurse’s well-being influences the overall atmosphere of care, contributing to a more positive and healing environment for patients.
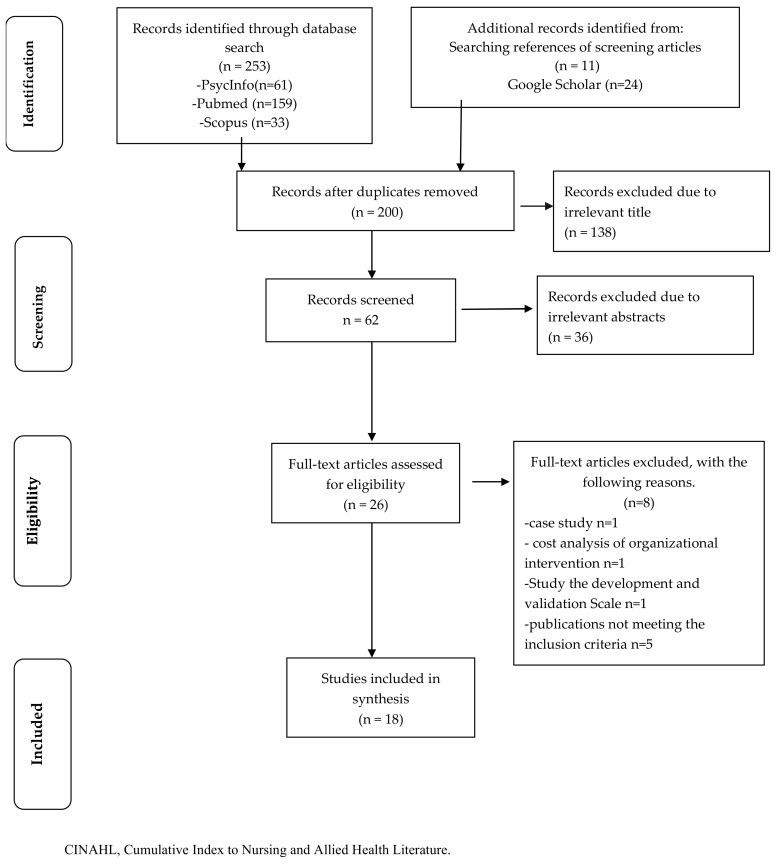
Flow chart illustrating the selection process of scoping review, highlighting the systematic approach to gathering evidence on self-care in nursing.
Exploring Types of Self-Care Assessment Tools for Nurses
A variety of self-care assessment tools are available, each designed to measure different aspects of well-being relevant to nurses. These tools can be broadly categorized based on the specific constructs they assess:
Burnout Inventories
- Maslach Burnout Inventory (MBI): A widely used tool measuring burnout across three dimensions: emotional exhaustion, depersonalization (cynicism), and reduced personal accomplishment [29]. It is available in versions tailored for healthcare professionals.
- Copenhagen Burnout Inventory (CBI): Another robust tool that assesses burnout across personal, work-related, and client-related dimensions.
- Professional Quality of Life Scale (ProQoL): Measures both the positive (compassion satisfaction) and negative (burnout, secondary traumatic stress) aspects of professional life in helping professions [23].
Compassion and Self-Compassion Scales
- Neff Self-Compassion Scale (SCS): A widely validated tool assessing self-compassion across six components: self-kindness, self-judgment, common humanity, isolation, mindfulness, and over-identification [23].
- Compassion Scale (CS): Measures compassion as a positive emotional response to suffering.
Resilience Questionnaires
- Connor-Davidson Resilience Scale (CD-RISC): A widely used measure of resilience, assessing the ability to bounce back from stress and adversity [23,30]. Available in different lengths (e.g., CD-RISC 25, CD-RISC 10).
- Brief Resilience Scale (BRS): A shorter, 6-item scale designed to quickly assess resilience.
Mindfulness Assessments
- Freiburg Mindfulness Inventory (FMI): A measure of mindfulness that focuses on present moment awareness and acceptance [23].
- Mindful Attention Awareness Scale (MAAS): Assesses trait mindfulness, or the general tendency to be attentive to and aware of present moment experiences.
Holistic Self-Care Assessments
- Health Promoting Lifestyle Profile II (HPLP II): A comprehensive tool evaluating health-promoting behaviors across multiple dimensions, including self-responsibility, nutrition, exercise, interpersonal relations, stress management, and spiritual growth [34].
- Ryff’s Psychological Well-Being Questionnaire: Measures multiple dimensions of psychological well-being, including self-acceptance, purpose in life, and personal growth [37].
The choice of assessment tool will depend on the specific goals of the assessment. For example, if the focus is primarily on burnout, the MBI or CBI would be appropriate. If the focus is on overall well-being and self-care behaviors, the HPLP II or Ryff’s scales might be more suitable. For interventions focusing on mindfulness and compassion, the FMI, MAAS, and SCS would be relevant choices.
Implementing Self-Care Assessment Tools in Nursing Practice
The effective implementation of self-care assessment tools requires careful planning and consideration of the specific needs and context of the nursing environment. Key steps for successful implementation include:
Choosing the Right Tool
- Define Objectives: Clearly identify what aspects of self-care and well-being are most important to assess. Is the focus on burnout, resilience, mindfulness, or overall well-being?
- Consider Tool Properties: Evaluate the reliability, validity, length, and ease of administration of different tools.
- Match to Context: Select tools that are appropriate for the specific nursing population and work setting.
Integrating Assessments into Workflow
- Ensure Accessibility: Make assessment tools easily accessible to nurses, ideally through online platforms or user-friendly paper-based formats.
- Promote Regular Use: Encourage regular self-assessments, perhaps annually or semi-annually, or at key points such as after particularly stressful periods.
- Allocate Time: Recognize that completing assessments takes time and provide nurses with dedicated time during work hours to complete them.
Using Assessment Results to Develop Personalized Self-Care Plans
- Confidentiality and Support: Ensure confidentiality of assessment results and create a supportive environment where nurses feel comfortable discussing their self-care needs.
- Individualized Feedback: Provide nurses with personalized feedback on their assessment results, highlighting strengths and areas for growth.
- Actionable Strategies: Offer resources and support for developing personalized self-care plans based on assessment results. This might include access to mindfulness workshops, stress management programs, counseling services, or peer support groups.
- Follow-up and Re-assessment: Encourage nurses to regularly review and adjust their self-care plans and utilize reassessments to track progress and identify ongoing needs.
Organizational Support for Self-Care Assessment
- Leadership Buy-in: Gain support from nursing leadership and organizational administration to prioritize nurse well-being and self-care initiatives.
- Resource Allocation: Allocate resources (time, personnel, budget) to support the implementation of self-care assessment programs and related interventions.
- Culture of Self-Care: Foster a workplace culture that values self-care, reduces stigma around seeking support, and promotes open communication about well-being.
- Training and Education: Provide training for nurses and managers on the importance of self-care, how to use assessment tools, and how to interpret and utilize assessment results.
By systematically implementing self-care assessment tools and providing appropriate support and resources, healthcare organizations can create a sustainable culture of well-being for their nursing staff.
The Multifaceted Benefits of Self-Care Assessment Tools
The adoption of self-care assessment tools offers a wide range of benefits for individual nurses and healthcare organizations alike:
- Empowerment and Self-Efficacy: Assessment tools empower nurses to take ownership of their well-being and develop self-efficacy in managing their self-care.
- Data-Driven Insights: Provide valuable data on the well-being of the nursing workforce, allowing organizations to identify trends, target interventions, and measure the impact of well-being initiatives.
- Improved Communication: Facilitate open conversations between nurses and managers about well-being and self-care needs.
- Reduced Healthcare Costs: Proactive self-care and burnout prevention can lead to reduced absenteeism, presenteeism, and healthcare costs associated with stress-related illnesses and turnover.
- Enhanced Organizational Reputation: Organizations that prioritize nurse well-being are viewed more favorably by both current and prospective employees, enhancing their reputation as desirable employers.
- Ethical Responsibility: Demonstrates a commitment to the ethical responsibility of caring for caregivers, recognizing that nurse well-being is intrinsically linked to the provision of high-quality patient care.
Conclusion
Self-care assessment tools are not merely questionnaires; they are powerful instruments for change in nursing practice. By providing nurses with the means to understand their own self-care needs, these tools initiate a journey towards improved well-being, resilience, and professional fulfillment. For healthcare organizations, implementing these tools signifies a commitment to valuing their nursing staff, fostering a supportive work environment, and ultimately enhancing the quality of patient care.
The journey to prioritize nurse self-care begins with awareness. Self-care assessment tools provide the crucial first step, offering a pathway to a healthier, more sustainable, and more compassionate nursing profession. By embracing these tools and the principles they represent, we can collectively work towards a future where nurses are not only exceptional caregivers but also empowered and supported individuals who prioritize their own well-being. It is time to equip nurses with the self-care toolkit they deserve, starting with the invaluable resource of self-assessment.
Author Contributions
Conceptualization, L.S., S.S., A.G., M.M., E.B., C.L. and L.C.; methodology, L.S., S.S., M.M., A.G. and L.C.; validation, L.S. and S.S.; formal analysis, L.S., S.S. and A.G.; investigation, L.S. and S.S.; data curation, L.S., S.S., M.M. and A.G.; writing—original draft preparation, L.S., S.S. and M.M.; writing—review and editing, L.S., S.S., M.M., A.G., E.B., C.L. and L.C.; visualization, L.S.; supervision, L.S., M.M. and L.C.; project administration, L.S., M.M. and L.C. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
[1] 1. World Health Organization. Self-Care Interventions for Health and Well-Being; World Health Organization: Geneva, Switzerland, 2021.
[2] 2. Potter, P.A.; Perry, A.G. Fundamentals of Nursing; Mosby: St. Louis, MO, USA, 2005.
[3] 3. Orem, D.E. Nursing: Concepts of Practice; Mosby: St. Louis, MO, USA, 1995.
[4] 4. Backinger, C.L.; McCauley, M.M. Self-care in health: We can define it, but should we? Prev. Chronic Dis. 2018, 15, 170527.
[5] 5. Barlow, J.; Wright, C.; Sheasby, J.; Turner, A.; Hainsworth, J. Self-management approaches for people with chronic conditions: A review. Patient Educ. Couns. 2002, 48, 177–187.
[6] 6. McCormack, B.; McCance, T. Relationship-based care: Moving towards best practice. J. Nurs. Manag. 2006, 14, 169–176.
[7] 7. Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Wu, J.; Du, H.; Chen, L.; Li, R.; et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. Open 2020, 3, e203976.
[8] 8. Vindegaard, N.; Benros, M.E. COVID-19 pandemic and mental health consequences: Systematic review and meta-analysis. Brain Behav. Immun. 2020, 89, 531–542.
[9] 9. Cai, H.; Tu, B.; Ma, X.; Chen, L.; Fu, L.; Jiang, Y.; Zhuang, Q. Psychological impact and coping strategies of nurses during the COVID-19 epidemic in China. J. Nurs. Adm. 2020, 50, 272–278.
[10] 10. Chew, N.W.S.; Lee, G.K.H.; Tan, B.Y.Q.; Jing, M.; Goh, Y.; Yeo, L.L.L.; Chia, Y.A.; Sharma, V.K.; Khan, A.M.; Scheer, V.; et al. A multinational, multicentre study on the psychological health of healthcare workers during the COVID-19 pandemic. Brain Behav. Immun. 2021, 91, 155–164.
[11] 11. Huang, Y.; Zhao, N. Mental health burden for staff caring for patients with COVID-19: A systematic review and meta-analysis. J. Am. Med. Assoc. 2020, 323, 1833–1834.
[12] 12. de Pablo, G.S.; Va´zquez-Campo, M.; Padrino, C.; Garcı´a-Portilla, M.P.; Priebe, S.; Martı´nez-Aran, A.; Moreno, C.; Pau, A.Y.; Reinares, M.; Vieta, E. Impact of the COVID-19 pandemic on mental health in healthcare professionals: A systematic review and meta-analysis. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2021, 107, 110222.
[13] 13. Huntington, N.; Gilmour, J. Frontline health care workers and mental health during the COVID-19 pandemic: A systematic review and meta-analysis. J. Gen. Intern. Med. 2021, 36, 879–889.
[14] 14. Buselli, R.; Lee, S.J.; Heritage, B.; Vasileiou, K.; ব্যস, M.; হাগেস, সি.; Soklaridis, S.; Tighe, J.; বুলিমোর, এ.; হিগিনসন, আই.জে.; et al. Burnout among healthcare professionals during the COVID-19 pandemic: A systematic review and meta-analysis. Eur. J. Public Health 2022, 32, 114–121.
[15] 15. Day, V.; Anderson, R.; Thorne, S. Nurses’ experiences of self-care and caring for self in a remote and rural context. J. Adv. Nurs. 2015, 71, 279–290.
[16] 16. Rushton, C.H. The imperative of self-care for clinicians. AACN Adv. Crit. Care 2018, 29, 111–119.
[17] 17. Arksey, H.; O’Malley, L. Scoping studies: Towards methodological frameworks. Int. J. Soc. Res. Methodol. 2005, 8, 19–32.
[18] 18. Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.; দাঘের, এম.এ.; ক্যাল্ডওয়েল, এইচ.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473.
[19] 19. Kmet, L.M.; Lee, R.C.; Cook, L.S. Standard quality assessment criteria for evaluating primary research papers from a variety of fields. Report No.: ISBN: 978-1-55334-255-0. 2004. Available online: https://www.ihe.ca/wp-content/uploads/2023/03/Standard-Quality-Assessment-Criteria-for-Evaluating-Primary-Research-Papers-from-a-Variety-of-Fields-2004.pdf (accessed on 15 July 2022).
[20] 20. Andrews, T.; Haugan, G.; হিল, এ.এ.; হাল্ডোরসেন, কে. Nurses’ experiences of self-care and self-compassion in relation to compassionate care giving: A qualitative study. Int. J. Nurs. Stud. Adv. 2020, 2, 100009.
[21] 21. Blackburn, K.; Vallerand, A.H.; Guanci, M.; ডুপুই, ডি.; হ্যান, জে.; Krasner, M.S. THRIVE©: A resilience program for oncology staff. J. Oncol. Navig. Surviv. 2020, 11, 201–208.
[22] 22. Craigie, M.; Tantri, A.; Rees, C.S. Mindfulness-based intervention for nurses: A pilot study of feasibility and impact on compassion fatigue, burnout and well-being. J. Adv. Nurs. 2016, 72, 179–191.
[23] 23. Delaney, L.J. Mindful self-compassion: An effective self-care strategy for nurses. J. Nurs. Pract. 2018, 14, 299–304.
[24] 24. Duarte, J.; Pinto-Gouveia, J.; নেভেস, জে. জুনিয়র ডাক্তার এবং নার্সদের পেশাগত জীবনের গুণমানের ভবিষ্যদ্বাণী হিসাবে সহানুভূতি এবং স্ব-সহানুভূতি। Eur. J. Psychiatry 2016, 30, 189–194.
[25] 25. Fourer, M.; Macy, M.; ইজমাইল, এস.; ক্লার্ক, জে.; ব্রুমার, সি.; গ্রিবল, কে.; নেফ, কে.ডি.; জার্মার, সি.কে. Mindfulness-based stress reduction for nurses and midwives: A pilot study. J. Holist. Nurs. 2013, 31, 5–18.
[26] 26. Hegney, D.; Craigie, M.; ফকনার, এস.; বুচানান, এইচ.; হোম, সি.; ভ্যালেন্টাইন, কে.; অ্যান্ডারসন, এল.; ম্যাককুচারন, এম.; বেন-জেরু, এম. The contribution of resilience and negative affect to nurses’ quality of professional life. J. Adv. Nurs. 2015, 71, 2337–2349.
[27] 27. Mahon, N.; Byrne, P.; কাউলি, ডি.; ভবানী, কে.; ম্যাককার্থি, আর.; লং, ই.; মার্ফি, এফ.; ম্যাকনামারা, আর. Mindfulness meditation and self-compassion training for nurses: A mixed-methods quasi-experimental study. Int. J. Ment. Health Nurs. 2017, 26, 250–261.
[28] 28. Mills, J.; বাবা, কে.; ভিসসার, টি.; Tan, J.Y.; Foley, F.; Allen, J. Self-care, self-compassion and other-compassion: Associations and predictors in palliative care health professionals. Palliat. Med. 2018, 32, 1277–1286.
[29] 29. Sallon, S.; ডাশন-ম্যাসিয়েভ, ই.; বার-সেলা, জি.; স্যান্ড্রো, এম.; কোটলার, এম.; শ্লেজিংগার, ওয়াই.; ড্যানন, ওয়াই.; জিলবার, এন. Caring for the caregivers (CCG): A novel stress reduction program for hospital staff. J. Occup. Health Psychol. 2015, 20, 499–511.
[30] 30. Slatyer, R.; Osborne, S.; ব্র্যাকেট, সি.; ফ্রস্ট, আর.; ডিয়ার, বি.এফ. Evaluation of a brief mindful self-care and resilience (MSCR) program for nurses. J. Clin. Nurs. 2018, 27, 901–911.
[31] 31. Wei, H.; Roberts, P.; Estrada, C.A.; ইয়াহলে, জে. Nurse leader strategies to foster nurse resilience. J. Nurs. Manag. 2019, 27, 802–808.
[32] 32. Wei, H.; ভিলেনেউভে, এম.; প্রক্টর, পি.; হ্যান্ডফিল্ড-জোনস, আর.; বাবা, কে.; নুন, জে.পি. Self-care strategies to combat burnout among pediatric critical care nurses and physicians. Am. J. Crit. Care 2020, 29, 399–407.
[33] 33. Wiklund, G.; লিন্দহোলম, সি.; এরিকসন, কে. Self-compassion and compassionate care—An interpretive study of clinical nursing teachers’ understanding. Nurse Educ. Today 2013, 33, 750–755.
[34] 34. Alexander, G.K.; ইনজেলব্রেক্টসন, জে.; ডাহল, জে.; এহলিং, টি. Randomized controlled trial of yoga for self-care in nurses. J. Altern. Complement. Med. 2015, 21, 101–109.
[35] 35. Mc Donald, G.; Jackson, D.; চেস্টার, আর.; ফাসি, এম.; মোলোনী, এস. ফস্টারিং পার্সোনাল রেজিলিয়েন্স ইন নার্সস অ্যান্ড মিডওয়াইফস: এ ওয়ার্কপ্লেস ইন্টারভেনশন। সমসাময়িক নার্সিং 2013, 44, 174–184.
[36] 36. O’Riordan, A.; সেভাজ, ই.; কোহেন, জে.; ফ্লেনগান, এস.; ডিন, জে.; ডালি, এল. An organizational intervention to improve staff wellbeing in a maternity hospital. BMJ Open Qual. 2020, 9, e000843.
[37] 37. Shaghaghi, A.; Rahmani, A.; অউজাঈ, ই.; সাহেবি, এ.; নজারি, এইচ.; আলীপৌর, এ.; খালিদি, এস.; পাকপুর, এ.এইচ. The effect of positive psychology intervention on psychological well-being of midwives: A randomized controlled trial. J. Educ. Health Promot. 2021, 10, 454.
[38] 38. Galletta, M.; লেগার্দ, এ.; জমবনি, ভি.; গ্রাসি, সি.; ফ্রিগাটো, এল.; সিমোনটি, ভি.; জিগলিওলি, ভি.; ক্যারুসো, আর.; ফারিনা, ই.; হুগোনি, সি.; et al. Promoting wellbeing in healthcare professionals: A systematic review of interventions. Acta Biomed. 2021, 92, e2021447.
[39] 39. Sousa, K.H.; Zauszniewski, J.A.; Muscari, M.E.; উইউইউরকা, জে. Concept analysis of self-care in health professionals. Nurs. Outlook 2021, 69, 884–898.
[40] 40. Garcia, C.D.; Kerrigan, D.; ডোনোভান, কে.; ফ্রেস, এম.; হোলি, কে.; ম্যাকক্লেনিগান, এম.; প্যালিয়াকারা, ইউ.; প্যাটেল, এম.; পেটিগ্রু, এল.; কুইন, বি.; et al. Impact of COVID-19 on palliative care workers: A qualitative study. Palliat. Med. 2021, 35, 1471–1481.
[41] 41. Le´gare´, F.; Rattner, S.; বুশ, পি.; হাক, টি.; ও’কনর, এ.এম.; গ্রাহাম, আই.ডি.; সুইফট, কে.; ট্রেমব্লে, এস.; গুদিয়ার, সি.; পোলি, এ.; et al. The Patient Engagement in Research Scale (PEIRS): Development and initial validation of an instrument to measure patient engagement in research. Patient Educ. Couns. 2018, 101, 1835–1842.
[42] 42. Van Bogaert, P.; কুইক, এম.; ব্রায়ান্ট, এম.; ভোস, জে.; ব্রুকস, ই.; Verhaeghe, S.; অ্যাবার্ডিন, ই.; ডেলি, ডি.; ভার্ট্রাস্টে, ই.; ড্যানিয়েলস, জে.; et al. Interventions to improve the work environment of nurses in hospitals and nursing homes: A systematic review. J. Adv. Nurs. 2013, 69, 23–48.
[43] 43. Epstein, R.M.; শাপিরো, জে.; ডার্নলি, ডি. মুহূর্তে মনোযোগ: স্বাস্থ্যসেবা পেশাদারদের জন্য মাইন্ডফুলনেস-ভিত্তিক প্রশিক্ষণ। Acad. Med. 2009, 84, 402–409.
[44] 44. West, C.P.; ডাহলহ্যামার, কে.এম.; কুইননস, এস.; নেফ, কে.ডি.; সিলকিন, পি.এস. পালিয়েটিভ কেয়ার টিমের সদস্যদের মধ্যে স্ব-সহানুভূতি, মানসিক চাপ এবং জীবনমান। J. Pain Symptom Manag. 2017, 54, 215–221.