Background
In the healthcare sector, the primary goal is to restore patient health, which heavily relies on the effective and efficient use of medical data for informed interventions.1 Implementing a robust healthcare data management system, complete with precise case definitions, is crucial for streamlining data retrieval,2 improving communication for clinical decision-making,2–8 advancing clinical research,9,10 and ultimately elevating the quality of healthcare services.11 Healthcare professionals are continuously striving to enhance data recording, distribution, monitoring, and the implementation of preventative measures to reduce illness rates.12 This necessitates consistent, complete, comprehensive, and accurate information, which is a growing area of focus within the healthcare industry.3
Healthcare facilities utilize both paper-based records (PBR) and electronic health record (EHR) systems to handle patient data. EHRs have become essential in modern medical care,13 revolutionizing healthcare service quality14,15 and increasing satisfaction for both clinicians and patients by facilitating informed decisions.8,16 The precision of EHR data allows physicians to accurately enter orders and assess clinical validity, thereby improving patient care standards.17 This capability is vital during diagnosis and treatment,15 offering benefits to both medical and legal practices.18
EHR systems come equipped with decision-support features like standardized checklists, alerts, predictive tools, and guidelines1 that encourage healthcare leaders and physicians to effectively use best practice alerts (BPAs).19 Research supports the shift from PBR to EHR systems in healthcare,17 although some reports indicate that EHR systems may be less adaptable for specific specialties like eye care recording.20
EHR systems offer readily accessible and transferable patient data,21 which aids in making accurate diagnoses and decisions22 by reducing access and usage time.1,2 BPAs and notification signals highlight crucial information and guide data sharing,23–25 alerting reviewers to potential adverse events (AEs) through easily identifiable displays.26 This enhances patient involvement in their healthcare27 and decision-making processes,28 fostering trust29 and confidence30 and helping to pinpoint specific adherence barriers.31 Furthermore, automated reminders via email, text, and phone can be sent to patients to encourage and improve adherence to treatment plans.32
Ineffective data management practices are often the root cause of recurring errors, injuries, or even fatalities,33 frequently stemming from illegible PBRs34 and mistakes during recording or transcription.35
EHR applications enhance the efficiency, reliability, safety, and overall effectiveness of patient care delivery.29 Therefore, implementing standardized policies, processes, and procedures for healthcare data management is vital for improving service quality and efficiency,34,37 eliminating wasteful activities,34 and ensuring significant improvements in safety and quality.16,17,23,34 This review aims to highlight the crucial roles EHR systems play in enhancing the quality of healthcare service delivery as essential client care tools.
Methods
This review utilized a comprehensive search strategy to gather relevant articles. Keywords including EHR, EMR, electronic health record, electronic medical record, medical data recording, medical data processing, medical data retention, medical data destruction, health care, patient care, animal data, and plant data were used in various combinations. Boolean operators “AND”, “OR”, and “NOT” were employed to refine the searches.
The search strategy specifically used was: [((EHR OR EHR[MeSH terms]) OR EMR) OR (EMR[MeSH terms]) OR (electronic health record) OR (electronic health record[MeSH terms]) OR (electronic medical record) OR (medical data recording[MeSH terms]) OR (medical data processing) OR (medical data processing[MeSH terms]) OR (medical data retention) OR (medical data retention[MeSH terms]) OR (medical data destruction) OR (medical data destruction[MeSH terms])] AND [((health care) OR (health care)[MeSH terms]) OR (patient care) OR (patient care)[MeSH Terms])]. Databases searched included PubMed, Google Scholar, and the Google search engine. Information extracted from the collected materials was then synthesized qualitatively.
Results
The search for published materials was conducted using PubMed (National Library of Medicine [NLM]), Google Scholar, and the Google search engine. EndNote® Version X5 for Windows was utilized to manage downloaded materials. Articles identified through EndNote were screened for relevance based on titles, abstracts, and full-text reviews. This screening process was independently performed by two reviewers to ensure eligibility. Out of 4,606 initially identified publications, 73 full-text articles published between 2013 and 2018 were selected for this review after rigorous screening and selection processes. The data from these materials were qualitatively synthesized to develop the insights presented in this review. The article selection process is detailed in Figure 1.
Figure 1.
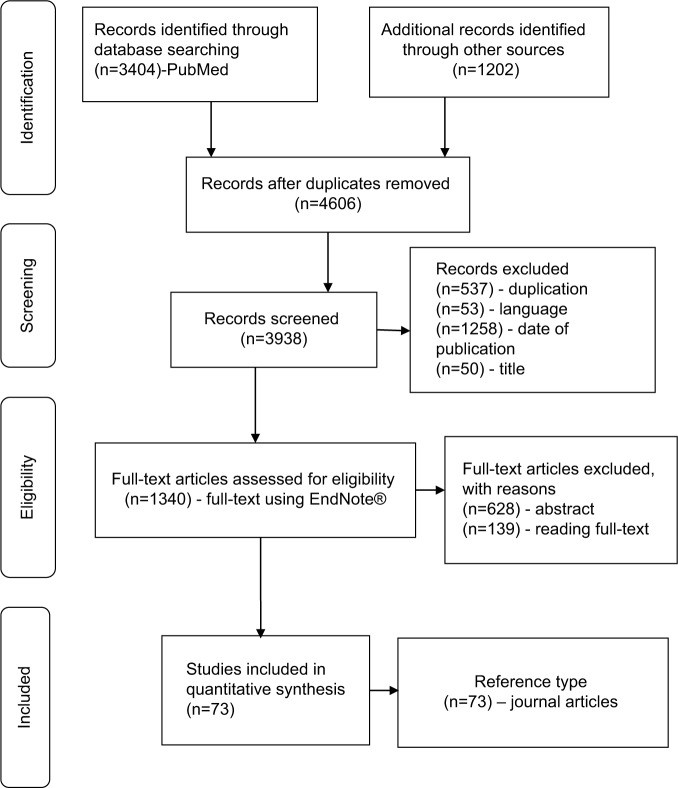 PRISMA flow diagram of article selection process
PRISMA flow diagram of article selection process
Discussion
Patient Healthcare Data Management Processes
The healthcare industry is fundamentally an information-driven sector; however, data recording practices and data protection regulations can differ significantly across hospitals and countries.38,39 Comprehensive healthcare data management policies must prioritize confidentiality and establish protocols to prevent data reconstruction after destruction, overseen by security personnel.
A robust document destruction policy should outline medical data retention guidelines and codes of practice, detailing the advantages and disadvantages of both destroying and retaining medical data.40 This is crucial for maintaining compliance and ensuring ethical data handling.
Benefits of EHR Implementation as Client Care Tools
Implementing EHR systems as client care tools significantly enhances service quality and patient safety. The integration of decision-support tools leads to fewer medical errors, increasing satisfaction among both clinicians and patients, which in turn encourages patients to actively seek healthcare services.
Currently, approximately 1,000 EHR applications are released monthly,42 aimed at improving performance,41,42 reducing clinician burnout, enhancing accessibility, ensuring regulatory compliance, maintaining data integrity, and increasing user satisfaction,41,43 all while maintaining acceptable safety standards.44
The successful implementation of EHR tools in large healthcare systems like those in the United States and the United Kingdom demonstrates their effectiveness in delivering quality patient care.45 EHRs are essential for leveraging modern information technology to improve healthcare service quality46 while adhering to medico-legal requirements.18
Easy access to EHR tools streamlines healthcare delivery,19,24 facilitates more accurate clinical decisions,22 and contributes to overall healthcare quality improvement and research outcomes47,48 at a reduced cost.49,50 These tools also ensure the secure transfer of healthcare data, meeting patient expectations,51 supporting continuity of care,11 and promoting medication adherence.52,53 Furthermore, EHR systems assist in achieving diabetes management goals and streamline service delivery with the support of non-physician staff.54
Data from EHR systems can be used to measure prevention efforts, process efficiency, and patient outcomes.55 High-quality EHR implementation enhances epidemic surveillance,56 reduces hospital stays,40 improves work efficiency33,40 by minimizing non-value-added tasks,34 helps achieve organizational goals,3 and supports timely decision-making while lowering costs.49,57 EHR systems reduce the time nurses and clerks spend accessing data, enabling quicker interventions.1 Ultimately, EHRs improve service quality and reduce costs.58 The key benefits of EHR systems include improved quality of care, enhanced continuity of patient care, increased efficiency, and a positive return on investment.50
Effective use of EHR systems enhances patient safety,48 builds trust, and increases patient satisfaction, orienting them towards reliable health information sources.59 Patients expect control over their data and want to be informed about data access.23 EHR tools can be customized to provide notifications and ensure the secure transfer of confidential patient data,33 requiring robust protection measures.60
The interoperability of medical information across healthcare institutions improves medical staff’s understanding of diseases, diagnoses, and decision-making processes.61 EHR systems facilitate automated disease surveillance and promote safe and effective healthcare practices.56
Challenges in EHR Implementation
Despite their advantages, EHR systems are often viewed as a “double-edged sword” because while they improve quality, they also introduce privacy and security risks.34 These concerns are significant for patients when it comes to transferring their healthcare data.23,33
Although EHR adoption rates are increasing, they remain low, especially in developing countries.46,62,63 Factors contributing to this low adoption include behavioral aspects (perceived lack of benefits,28 low confidence,64 dissatisfaction,59 physician resistance,65 insufficient stakeholder interest,49 and limited awareness of advanced systems),60,66 technical challenges (interoperability issues,64 lack of financial support or incentives,49 and inadequate technology infrastructure),47 legal barriers (absence of a legal framework64 and comprehensive national EHR policies),47 socio-demographic factors (physician age and education level),59 practice-related issues (high skill requirements28 and insufficient training),67 and knowledge gaps (poor awareness).64
A Delphi study identified barriers to EHR implementation in medical practices, highlighting both intrinsic (behavioral and cognitive) and extrinsic (economic and technological) obstacles that healthcare providers face when considering investing in EMR systems.50
Telehealth and Remote Healthcare Services
Traditional telephone services paved the way for modern telemedicine. Advanced electronic communication applications now enable remote healthcare operations. Despite global efforts to reduce medical errors, healthcare professionals still make mistakes during manual data processing, including recording errors and delays in data entry.35 Medical data-related errors are frequent and costly. When implementing new healthcare technologies, it is essential to consider the social, spiritual, psychological, and ethical dimensions, as well as technical feasibility, and involve all stakeholders in the planning and implementation process. While PBR systems are more prone to errors, simply switching to EHRs does not guarantee accuracy.34 Therefore, efficient processing, use, and storage of medical data are crucial for both clinical and public health decisions.
Future Directions in Client Care Tools
The successful implementation of EHR systems depends on factors related to people, processes, and products.11 Stakeholders benefit from systems that protect patient needs and ensure privacy.24 Access to accurate and complete clinical information is fundamental for effective decision-making.69 EHR decision-support tools, such as BPAs, are designed to integrate behavioral health needs with healthcare operations and improve patient experiences,36 for example, in managing alcohol use disorders.30 These systems can update patient conditions to provide recommendations for medical tests, potential diagnoses, and treatment plans.69 Research shows that EHR “active choice” prompts significantly increased influenza vaccination rates and the use of colonoscopy and mammography screening services.8
Voice input applications can be utilized to transcribe doctor’s dictations, streamlining the collection, indexing, storage, and retrieval of medical information.17 However, studies suggest that while EHRs enhance service delivery, they may not always foster a collaborative team culture among professionals.70
The growing adoption of EHR in healthcare builds trust and offers opportunities to monitor admissions, diagnoses, and outcomes, informing public health policy and service delivery.58 EHR vendors should be encouraged to integrate social knowledge networking features into their systems.71
Researchers have identified areas needing further investigation. One national study indicated higher EHR adoption rates in rural practices compared to urban settings, reversing previous trends.72 Another study highlighted the importance of considering patient behavior when using EHR tools during patient interactions to enhance patient engagement.73 These findings suggest a need for behavioral scientists to address these specific patient-related concerns.
Conclusion
Medical data processing is a core task for healthcare professionals. Computerized physician order entry systems with decision-support features reduce preventable medical errors by providing built-in memory aids. Automatic notification alerts enable timely and appropriate interventions, ensuring safer and more efficient healthcare. The design of electronic healthcare technology must adhere to predefined standards and guidelines to guarantee data confidentiality. User-friendly technologies are essential for the efficient and timely transfer of healthcare data, ultimately improving patient care and meeting the needs of both patients and healthcare organizations.
Abbreviations
AEs Adverse Events
BPAs Best Practice Alerts
EHR Electronic Health Record
EMR Electronic Medical Record
NLM National Library of Medicine
PBR Paper-Based Record
Footnotes
Author contributions
All authors contributed towards data analysis, drafting and critically revising the paper, gave final approval of the version to be published and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.


